Care Pathway Analysis to Inform the Earliest Stages of Technology Development: Scoping Oncological Indications in Need of Innovation
Section Editor: Agnes Benedict
Scholte M, Heidkamp J, Hannink G, Merkx MAW, Grutters JPC, Rovers MM. Value Health. 2023;26(12):1744-1753.
Many medical innovations are applicable across several disease areas. Identifying where they would make the biggest contribution to overall patient health is an important process that innovators, public and private funders of research, and payers of health services go through. The assessment process is sometimes referred to as development-focused health technology assessment, or early health technology assessment. While many organizations do this more or less transparently and explicitly in order to prioritize disease areas for products, few standardized methods have been proposed for this. An article by Boutell et al published in the International Journal of Technology Assessment in Health Care proposes care pathway analysis as one approach.
Care pathway analysis is a systematic process to evaluate and improve the efficiency and quality of patient care. It involves mapping out and visually presenting the sequence of events, interventions, and resources required to deliver a specific type of care or manage a particular health condition. By analyzing the care pathway, healthcare providers can identify variations in practice, potential bottlenecks, and opportunities for improvement. This analysis helps in optimizing resource allocation, reducing unnecessary costs, enhancing patient outcomes, and standardizing care delivery across different settings.
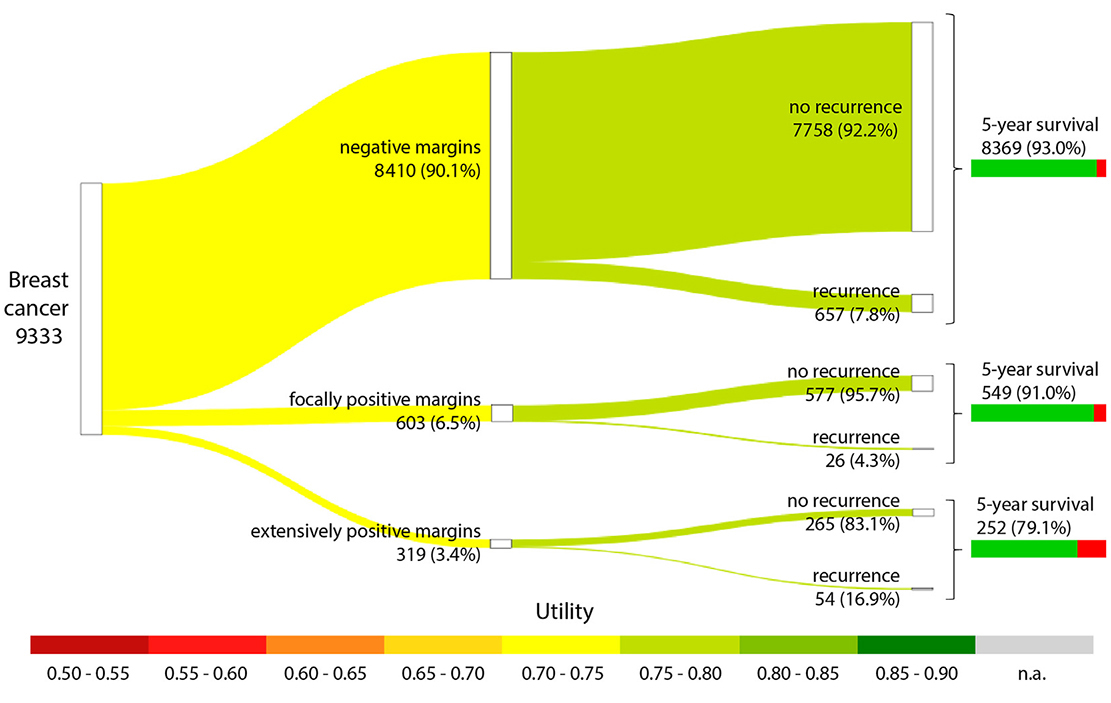
In their recent paper published in Value in Health, Scholte et al set out to explore a care pathway approach in the context of innovation. Specifically, their paper investigates which cancer areas would benefit most from most newly developed advanced imaging techniques that are aimed at identifying tumor tissue and detecting positive margins during surgery (eg, optical coherence tomography). Their key outcome is an “effectiveness gap”—the difference between the ideal outcome (complete resection for all) and the status quo (with current rates of positive and negative margins). The magnitude of the effectiveness gap is then used to identify the areas that would benefit most from advanced imaging techniques.
The care pathway analysis included semistructured interviews that were conducted at multiple timepoints: before the study to find out about margin assessment and identify cancer areas where margin assessment is important; and at the results stages to externally validate the resulting pathway diagrams, data inputs, and results. A very simple general model was specified that would be applicable for each cancer area. It captured annual number of patients impacted, the groups of patients with and without complete resection, and the implications of complete versus incomplete resection, in terms of quality of life, recurrence, and 5-year overall survival. A Sankey diagram was constructed to graphically represent the pathways with several layers of information (see the example for breast cancer in Figure 1).
Figure 1. Care pathway analysis for breast cancer.
Models were parameterized based on a Dutch registry for patient numbers and surgery results, and desk research on health utilities, recurrence, and survival rates, covering 6 cancer areas: breast cancer, glioblastoma, bladder cancer, prostate cancer, pancreatic cancer, and oral cavity cancer.
The authors presented results for each cancer in terms of recurrence rates in utility values and in 5-year overall survival in a simple transparent table. Authors stopped short of creating a summary metric for the effectiveness gap and no attempt was made at analyzing uncertainty.
Nevertheless, by using a comprehensive and systematic assessment of existing care pathways with a simple model, they allow comparisons across conditions. The models are easy to update with new information or to incorporate major changes (eg, emergence of curative therapies). By comparing the effectiveness gaps, the potential for maximizing health benefits of innovative solutions can be highlighted from several perspectives.
Even with limitations, such formal exercise could provide a more informed approach to prioritize scarce research funding and investment for both public and private funders of research.

