HU Shanlian, MD, Professor of Health Economics, School of Public Health, Fudan University, Shanghai, China
Introduction
This is based on an interview with Professor Shanlian Hu in the Department of Health Economics, School of Public Health, Fudan University in China and a Journalist of China Medical Insurance, published on 28th October 2021.
The basic contradiction of Economics is that the resources are limited and the demand is unlimited. There is, therefore, a need for effective and prioritized allocation of resources. Health Economics is a sub-branch of Economics intersecting the health
sector. Studying economic law of health development can effectively allocate health resources, improve the fairness and efficiency of the healthcare system, reduce costs, and promote accessibility. The ultimate goal is to improve the people’s
health status.
In the past two years, with the continuous strengthening and deepening reform of the health security system in China, health economics and outcomes research (HEOR) has played an increasingly important role in the adjustment of the medical insurance
reimbursement list, innovative drugs’ price negotiation, and the procurement of medicines and medical consumables, having undergone practical applications in these areas. But beyond this, can the reform of the health insurance system be
improved by using HEOR? What direction can HEOR play a greater role in the future? The following conversion will attempt to answer these questions.
What are the special features of the application of economics in the field of healthcare compared with other fields?
Compared with other fields, the application of economics in the field of healthcare has many particularities in the health service market and health products. For example, the prevention and treatment of many diseases have externalities; health insurance
has the characteristics of third party payment, and it has information asymmetry between doctors, patients and health insurance schemes. Consideration should also be given to ensuring equitable access to health services for the population, sustainable
financing of healthcare, and prevention of regulatory failures. In the area of health services, both the basic medical needs and the basic medical insurance services are required to meet the needs of the general public as well as the needs at different
demand levels, including public goods and preventive health service which serve the population with extensive benefits. Under the background of the new era of COVID-19 pandemic, the concept of “Fairness first” should be emphasized between
“Efficiency” and “Fairness.”
How to balance the “Public attribute” and “Economic attribute” of health insurance in this process?
In the reform of the health system, it should always adhere to the principle of “Protecting the basic level, strengthening the grass-roots facilities and establishing the mechanism”. The high-quality development of healthcare and medical insurance
should always follow this principle. Although China is already the second largest economy in the world, its GDP per capita is only about 12,500 US dollars in 2021. Although the coverage rate of medical insurance in China has stabilized above 95%,
the level of total insurance premium still varies greatly among regions. Therefore, the medical insurance funds should be allocated into the basic medical items, to ensure that the majority of the people have access to the “most basic”
medical and health services. For those special medical services, there is a need to rely on market forces to develop commercial medical insurance and private medical institutions to meet the needs of a small number of high-income people.
What economic principles have been applied in the reform of the medical insurance system in China?
Firstly, the basic medical outpatient insurance system is recently being established, reflecting the economic principles of social medical insurance. The principles of basic medical insurance are solidarity, mutual assistance and risk sharing better than
the original medical savings account using for outpatient insurance in China. The healthy people help the sick, the younger help the elderly, the rich help the poor. The personal savings accounts and household savings accounts, while increasing awareness
of personal costs, are by no means the way forward for basic healthcare. The health insurance funds contributed by each insured are pooled together to create a pool of funds to protect against the financial risks resulting from an individual’s
risk of illness. This is why the system of outpatient personal accounts should be transferred to the establishment of outpatient coordinating funds, reflecting the economic principles of social health insurance.
Secondly, medical insurance plays a role of strategic buyer in strengthening the centralized purchasing and price management of medicines and medical consumables. The National Healthcare Security Administration (NHSA) represents the interests of the vast
number of insured and intends to reduce the overpricing of medicines and medical consumables, especially reducing wholesaler margin in the sales of the products after ex-factory price. According to international practice reported by WHO, generally
the wholesale mark-up rate is between 3% and 8%. However, in the original business environment of China the multiples of mark-up are surprising, which is the main factor causing the high prices. Under the current situation of centralized procurement
with quantity, quality is the first, then, volume and price are linked by means of market competition. A given amount of market share (50%-80%) based on the number of tenders is used for centralized procurement. The Medical Insurance Fund provides
payment in advance for the hospitals which ensures the turnover of the capital of pharmaceutical enterprises, and greatly improves the efficiency of production. The results include many advantages that the prices of medicines and medical consumables
are reasonably reduced; the medical insurance fund is relieved; the medical cost of hospitals and patients are reduced; and the sales volume of pharmaceutical companies is increased.
Thirdly, the payment system for medical insurance has been reformed. The way of payment from fee-for-service system changed to the diagnosis-related group (DRGs) and big data diagnosis-intervention packet (DIPs) scheme under the hospital global budget
control. Both are prospective payment methods based on disease scores. This way not only controls the unreasonable increase of medical cost and improving the efficiency of medical insurance fund, but also standardizes medical behavior and promoting
medical quality.
Can you give some examples to illustrate the practice of HEOR in the field of healthcare system reform?
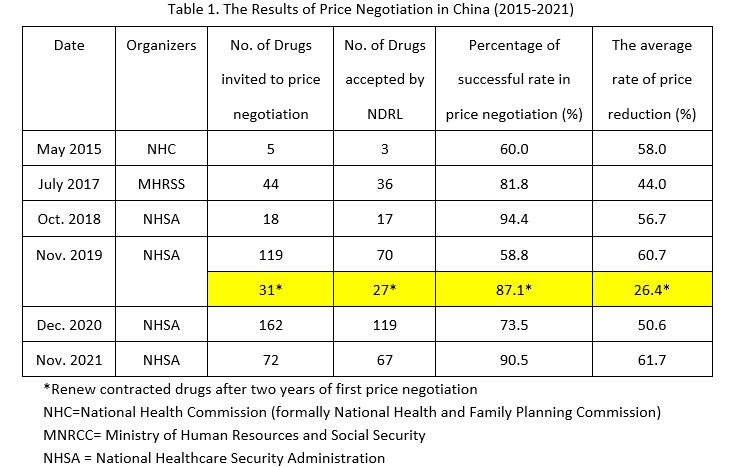
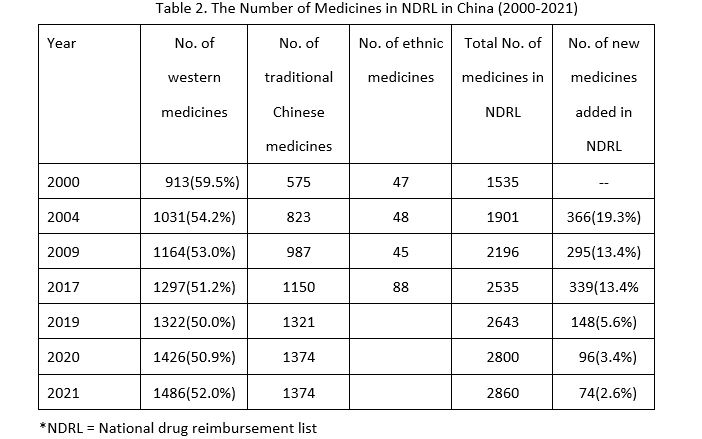
The price negotiation of innovative drugs has been organized and carried out by the NHSA since 2018. The health insurance sector plays a role of strategic purchaser, representing the interests of populations and patients to guide the reasonable price
reduction of the medicines with patents and exclusive varieties in higher prices, which will be finally included into the medical insurance drug reimbursement list.
After several years of practice, at present, the content of the submission guidelines is increasingly completed in the proposed negotiations of new drugs and renewed contract negotiations process. The Expert groups of Comprehensive Evaluation, Pharmacoeconomic
Evaluation, and the Health Insurance Fund Measurement, all play the role of “Escort”. Many important research methods and tools for pharmacoeconomics evaluation and health technology assessment have been applied, such as evaluation of
drug innovation, calculation of reasonable price range and forecast of drug price, selection of comparators, incremental cost-effectiveness ratio, budget impact analysis, international and domestic reference price, pricing of new indications, etc.
Moreover, a consensus building of conceptual and methodologies has been reached among the health care sector, pharmaceutical companies, experts and evaluation agencies. In light of China’s current level of economic development and huge market
potential, the aspect of price adjustment should be judged based on the rationality of the price of the declared drugs according to whether the ICER value met the threshold of China’s GDP per capita. The lowest international reference price
is chosen as the starting point of price negotiation.
From the present peer-review negotiation model what aspects do you think can be improved in the future?
Price negotiation in medical insurance is a multi-disciplinary work, which needs the combination of experts from physicians, pharmacists, health economists, medical insurance authorities, etc. Many countries have set up special health technology evaluation
agencies to provide evidence for government decision-making. The specific work shall be undertaken by third party professional institutions. The government organizes some evaluation committees to hold regular meetings and master plan to ensure the
continuity of the evaluation task, which can greatly save the management cost.
On the other hand, from the international experience, it is necessary to establish a set of scientific norms, fair and transparent pharmacoeconomic evaluation guidelines and standards.
Some people have called for the Health Insurance Fund to take on more responsibilities for encouraging innovative drugs in the national drug reimbursement list. How do you find a better balance between the “basic” nature and scientific innovation?
It should be made clear that it is the responsibility of the whole society to encourage drug innovation. In China, the Development and Reform commission, the Ministries of Finance, Science & technology, Industry & information, should take the
responsibility of leading role to guiding and organizing the R & D and production of innovative drugs. The Department of Health is responsible for the clinical application and allocation of innovative drugs. Finally, when it comes to the market
access, the NHSA needs to play a strategic purchaser role according to the fund’s affordability. To promote the development of pharmaceutical industry, some innovative drugs that can meet the needs of basic medical insurance will be included
in the reimbursement list through price negotiation, so that they can get reasonable returns as soon as they come into the market.
Based on the actual situation of China’s medical insurance system, what innovative payment mechanisms for medical products are worth learning from international society, especially for those with high-price products which launch to the Chinese market in a very short time with an unclear clinical value, but might fill a clinical gap?
There are many innovative payment mechanisms for innovative medical technology or medical products in the world, but it is necessary to consider the actual situation of China when learning from international experience. Especially for those cell therapy,
gene therapy and other one-time treatment need to pay a high cost for advanced therapy, annuity payment method can solve the problem. But this needs to have a good credit system, the consummation tax revenue system and the property mortgage system.
Another example is the “risk- sharing agreement”. Under this payment mechanism, if the clinical curative outcomes have not achieved the anticipated effect, the pharmaceutical enterprise needs to bear part of the drug cost. But it requires
a robust information system to support contract execution, clear clinical end point metrics, and information that can be easily accessed by healthcare providers, hospitals, drug companies, and patients. It is hard to do it if you are Information
asymmetry.
One of the most common and most likely to be implemented conditionally is to establish a program for coverage with evidence development (CED). Because there are many innovative drugs only from the preliminary phase II clinical results or single
arm trial, there is no gold standard for reliable results from a phase III randomized controlled double-blind trial so that a further result of real-world study needs to be collected and submitted to the medical insurance authority when the
contract is renewed. In addition, a more common approach is to set up a “CAP” on the number of people treated for an innovative drug or the total cost of reimbursement from the health insurance budget in advance, if it exceeds
the ceiling to be paid by pharmaceutical companies, this ensures that the risks of health insurance spending are manageable.
The pilot of price reform of medical service will be launched soon, how can health economics be applied to it?
With the development of medical technology, it will be more difficult to set the pricing for complex medical service items. For example, many companion diagnostic methods associated with genetic testing and personalized medicine. It requires the
establishment of special items in fee-for-service, or it should be included in the bundled payment. Another example, such as CAR-T cell therapy, which requires not only clinical blood drawing, cell isolation, but also gene editing or cell
culture in a lab. The pricing of such therapies are being explored. It will require the government to conduct pilot studies to develop a set of rules and standards. In practice, we can understand the whole production process, calculate the
discount of various fixed equipment, direct cost, indirect cost and profit rate to forming “cost plus pricing” method, then according to the value of innovation to give “value-based pricing.”
Pricing is both a science and an art. The right way is to control the unreasonable medical expense, and can indirectly encourage the innovation and development of medicines. The prices of basic medical services should be at a low level, but there
are many advanced medical technologies such as robotic surgery, 3D printing imaging, interventional therapy, cell therapy, ubiquitin-mediated targeted protein degradation (PROTAC) and the development of new vaccines, the pricing of those projects
also needs more domestic and international experience.