Wearables: Making a Mark in Digital Health
The wearable devices market is expected to grow at a compound annual growth rate of 18% from now until 2026.1 While interest in wearables may have originated in consumer-oriented wellness products, increasing interest in health applications, especially during the current COVID-19 pandemic, is driving market growth. In addition, wearables’ miniaturization, reliability, and accuracy are expanding possible healthcare use cases.
Susannah Fox, former Chief Technology Officer at the US Department of Health and Human Services; Laurie Orlov, founder of Aging and Health Technology Watch; Dave Albert, MD, founder and Chief Medical Officer, AliveCor; Vivian Lee, MD, PhD, MBA, President, Health Platforms, Verily Life Sciences; and Jessica Mega, MD, MPH, cofounder and Chief Medical and Scientific Officer, Verily Life Sciences, shared their thoughts on the current wearables market, how these devices are changing research, and how health economics and outcomes research may support this growth.
The Changing Nature of Wearables
The first wearable devices or “wearables” arrived in the 1920s when a British man named John Harwood was awarded the first patent for a pedometer. Today, wearables refer to small electronic mobile sensors incorporated into daily wear items (watches, eyewear, earbuds, rings) that collect biometric or activity data (Table 1).
Table 1. Types of wearable sensors and targeted measurements.
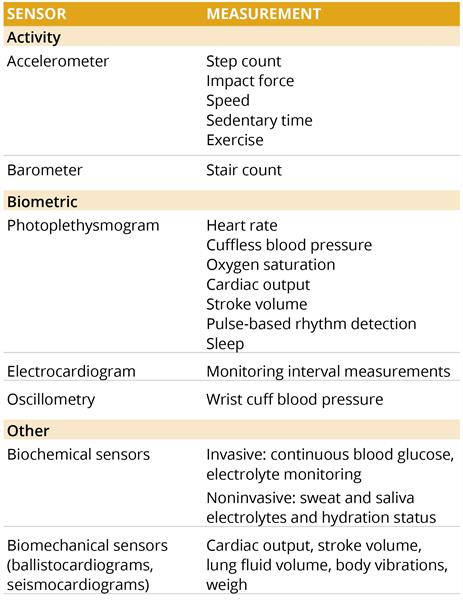
These devices capture a broad array of patient-generated health data: vital sign measurements (heart rate, skin temperature), physical activity (steps, duration of movement), sleep patterns, continuous glucose monitoring, and health events such as falls, strokes, and atrial fibrillation. In addition, new devices are in development to detect depression and other mental health conditions. Wearables are often paired with a companion smartphone app allowing patients, providers, or other stakeholders to review data on health trends and events.
Evolving Use Cases for Wearables
Wearable devices have the potential to collect large quantities of continuous patient-generated health data in real time—data that could inform clinical decision making and provide earlier diagnoses. For years, wearables have provided consumers with the activity data needed to reach their health goals such as weight reduction or blood pressure management.
Wearables can deliver important “between visit” data to providers, offering critical insight into a patient’s specific treatment response and health status. Not only can these devices assess whether a product is working as intended, but they can also alert case management of health events that may warrant intervention.
With the expanded use of telehealth due to COVID-19, wearable data allow remote providers to diagnose and monitor these patients. They have also enabled the smooth continuation of managing clinical trial patients by enabling trial participants to provide their trial data without a face-to-face visit.
Wearables could also become the foundation for some outcomes-based agreements, providing payers with additional data to support reimbursement. Payers must often make reimbursement decisions with incomplete information. Small clinical trial populations, short-term data due to accelerated approval, suboptimal outcomes measures, and other data gaps create uncertainty for payers. Orphan drugs for rare diseases (especially in pediatric populations), high-cost curative therapies, and conditions with high unmet need often enter the market with limited data to reassure payers that these therapies can achieve clinically meaningful improvements in the payer’s population. Wearables may help fill this data gap, providing the additional evidence payers need to determine whether the clinically proven outcomes demonstrated in clinical trials are observed within their population.
The Growing Influence of Consumers
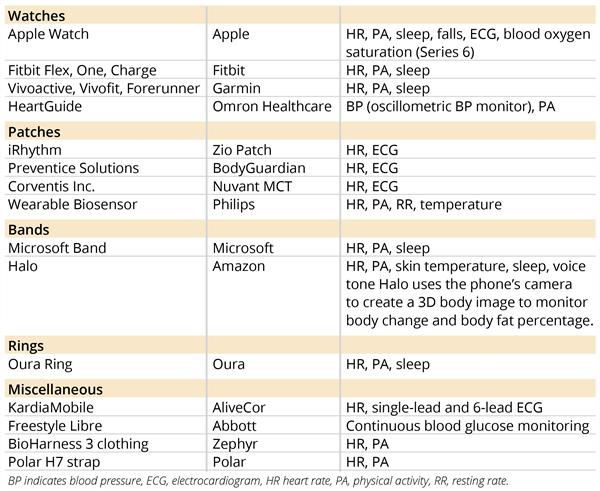
The use of wearable devices has more than tripled in the past 4 years,2 bringing new products and manufacturers into the market. While consumer electronics companies have dominated the wearables market, new and expanding opportunities for wearables in health services and clinical trials have led to a growing presence of healthcare and device companies. Table 2 lists some of the key companies currently in this market.
Table 2. Wearables 2021: Top products, producers.
Miniaturization Leading to More Use Cases
Thanks to higher quality, consumer-grade sensors, wearables continue to shrink in size, expanding their possible uses. For example, new smart patches can measure temperature, heart rate, blood sugar, and other vital statistics as (or more) effectively than other wearable technologies. They can also remotely administer medication, such as insulin for diabetic patients.
The performance gap between medical- and nonmedical-grade wearables is closing with improved sensor accuracy potentially expanding opportunities for these miniaturized devices. And with advances in miniaturization enabling device makers to integrate sensors into discrete, nearly invisible wearables, patient acceptance may also increase.
Putting Data in Patients’ Hands
The popularity of consumer electronics means millions of individuals now own the technology that can help them engage more fully in personal health monitoring. For example, a 2019 Pew Research Center study found that 21% of US adults surveyed reported regularly wearing a smartwatch or fitness tracker.3 By 2022, more than 1 billion wearables are expected to be in use globally.4
Wearables place patients at the center of their health data-collection process. Continuous tracking of activity levels, sleep patterns, heart rate, or even body temperature could motivate patients to improve their health habits. While patients have traditionally taken a more reactive approach to their health (pursuing care when they feel sick or in pain), new wearable devices can now alert patients of potential concerns. And as more patients gain access to their real-time health data, better health outcomes may be on the horizon for millions of patients.
Susannah Fox, former Chief Technology Officer, the US Department of Health and Human Services, Washington, DC, USA has long focused her research on how people use emerging technologies to pursue diagnoses and advocate for treatment. She supports the growing use of wearables, especially their role in furthering the citizen science or community science movement.
Wearables may help fill this data gap, providing the additional evidence payers need to determine whether the clinically proven outcomes demonstrated in clinical trials are observed within their population.
Fox noted that wearables support the possibility of “N of One” studies where individuals can solve their health questions. “Wearables can be very useful tools for people who have a theory about their health.” She views these individuals as pioneers, many of whom are in the rare disease space, engaging in “peer-to-peer healthcare” and sharing insights built from their data. Fox noted such initiatives are not new, with 14 past Nobel Prize winners having been “self-experimenters,” seven of whom won prizes for their work.
In her view, these pioneers are not unlike other tech innovators. “What they’re doing now is going to be widespread in 5 or 10 years.” Given the initiatives these early adopters have shown in their use of wearables, Fox hopes business leaders and policy makers follow the pioneers and support their collaborative approach to health data.
Fox acknowledged, however, the spectrum of accuracy among these tools. Currently, clear guidance regarding which apps gain featured promotion remains limited and consumer popularity seems to take precedence (see related piece, “Navigating the Digital Mental Health Landscape: One Mind PsyberGuide” published elsewhere in this issue). As a result, she proposes some third-party validity tests instead of the current approach whereby citizen scientists do those validity tests themselves.
However, Fox applauds the work of these pioneers as they break new ground for large entities (pharmaceutical companies, other healthcare companies) to follow.
Engaging Older Patients
While wearables with actionable health information can help motivate individuals and help patients gain control over their health, they are only effective when worn. Although wearables’ data could prove valuable in helping older patients manage chronic conditions to identify health events, the wearable market for older adults is in its infancy. Recent data show wearable acceptance among older individuals lags far behind that of younger citizens.
Laurie Orlov, founder of the blogspot, “Aging and Health Technology Watch”, is a strong proponent of wearable use in older adults. She recently published, “The Future of Wearables and Older Adults 2021,” in which she reviewed the benefits wearables offer older patients and the challenges of expanding adoption within this population.5
Wearables place patients at the center of their health data-collection process. Continuous tracking of activity levels, sleep patterns, heart rate, or even body temperature could motivate patients to improve their health habits.
Orlov sees significant value in wearables as monitoring devices for older adults and in their ability to supply data needed to refine treatment decisions and avoid possible over-medication of these patients. For example, she recounted how patients who experience office anxieties might have elevated blood pressure recordings during an office visit. These elevated readings could result in medications prescribed at dosages higher than may be necessary. By providing potentially more accurate trend data, wearables may improve prescribing practices.
She believes wearables may help detect disease progression at an early stage, possibly avoiding health events and related costs. For example, wearables could reveal early onset stroke symptoms or detect disease progression. Orlov highlighted how wearables might benefit patients with Parkinson’s disease, detecting changes in their condition outside infrequent clinic visits. Also, wearables might soon be able to identify early dementia symptoms or alert providers of a patient’s fall.
However, Orlov notes wearables only benefit patients when used consistently and correctly. As yet, acceptance of these devices among older adults has been slow. She notes that wearable markets, particularly for older adults, are in their infancy with only 20% of that segment of the population routinely using them, according to AARP.5
“Most of the progress in this space is happening outside the hospital and outside the doctors’ practices, driven by consumer tech companies.” — Laurie Orlov
She suggested some of this delay may be due to design issues, such as a small user interface compared to a smartphone. Older users may struggle to read status updates on their wearable devices. In addition, alerts may be too quiet for patients to hear. Consumers are already familiar with voice-based devices in consumer products, so incorporating voice-based activity into health wearables may be a possible remedy for difficult-to-read interfaces. Nevertheless, Orlov hopes that as design improves, wearables will become a standard part of the daily lives of older adults.
“As the data become available and validated, there will be more interest in wearables,” said Orlov. “For example, today there are studies underway comparing the efficacy of care for a person with a wearable and without a wearable.”
Orlov noted the importance of consumer electronics companies. “Most of the progress in this space is happening outside the hospital and outside the doctors’ practices, driven by consumer tech companies.”
Finding Clinical Value in Mountains of Data
A crucial part of improving patient outcomes is timely clinical intervention. High-quality patient-generated health data may provide early indications of worsening health. However, navigating through the mountains of trend data created by wearables remains challenging.
Dave Albert, MD, founder and Chief Medical Officer, AliveCor, Mountainview, CA, USA recognizes that we are in the early days of turning data into clinically meaningful insights and actions. But he notes that research shows that monitoring drug effects with wearables could improve clinical outcomes and reduce costs.
“We might be improving clinical outcomes, but we also might be improving financial outcomes. And that’s good for the patient and everybody else.” — David Albert, MD
Albert recounted a recent study by Labreck, et al, that demonstrated how wearables could reduce health services utilization and costs among patients starting sotalol (a class III antiarrhythmic).6 Given sotalol’s risk of QT prolongation, the US Food and Drug Administration requires monitoring new patients in an inpatient setting. However, with hospital capacity strained due to COVID-19, inpatient monitoring of patients during sotalol loading places an undue burden on hospital resources. The authors reported that the average sotalol loading cost of patients monitored with an AliveCor Kardia® wearable device in an outpatient setting was significantly lower than patients undergoing inpatient loading ($886.30 versus $7571.76, P <0.001). Said Albert, “We might be improving clinical outcomes, but we also might be improving financial outcomes. And that’s good for the patient and everybody else.”
He highlighted another significant benefit of expanded use of these products; improved access to health services. Wearables may help patients in remote or underserved regions receive ongoing medical care without hospitalization.
Albert noted that to improve patient outcomes, the artificial intelligence within the devices must perform with diagnostic sensitivity, specificity, and predictive accuracy (positive and negative). However, he emphasized that multiple stakeholders hold wearable producers, such as AliveCor, to high performance standards. “We are validated not only by the regulatory bodies but by the clinicians themselves.”
Empowering Patients as Coproducers of Health
Vivian Lee, MD, PhD, MBA, President, Health Platforms, Verily Life Sciences, Boston, MA, USA, sees wearables redefining how we view health outcomes. She notes that health outcomes have been defined traditionally by measures having more to do with processes than clinical states, such as administrative claims data. “They have very little input from the patients themselves,” she said.
“We are generating mountains of data. We don’t know what’s important yet clinically.” — David Albert, MD
She argues that wearables can change this approach to defining health outcomes. “Now we have a completely different way of thinking about health outcomes and about the quality of health measured. Not in terms of these processes or checklists (Did we avoid an infection? Did we avoid something bad happening to you?), but in terms that are meaningful to the individual patients. How is their quality of life? Are they able to engage in the activities that they want to engage in? Have they been able to lose the weight? Or manage their blood pressure? Or get through a pregnancy?”
She also sees wearables changing how we view health production. “We were trained in medical school that we, as doctors, were primarily responsible for your health.” She continued, “While in some settings, such as operating rooms, the doctor is mostly producing your health. But for most of the things that matter in our health, most takes place outside of the hospital or clinic: how you exercise, what you eat, how you sleep, your ability to comply with medications.”
Wearables and related software help individuals engage and coproduce their own health. “I think (this) is a fundamental mind shift that we’re seeing that we’re just participating in the earliest stages now.”
Providing a Nuanced View of Health and Health Outcomes
Jessica Mega, MD, MPH, cofounder and Chief Medical and Scientific Officer, Verily Life Sciences, Boston, MA, USA sees wearables as providing a more nuanced view of health outcomes. To Mega, these devices allow the capture of both the quantitative and qualitative aspects of many conditions. As an example, Mega noted that wearables might capture 2 different aspects: duration and quality of sleep. Or for Parkinson’s patients, wearables might quantify different parts of movement: the number of steps and the quality of ambulation.
Mega emphasized the importance of wearables data in helping researchers to observe variation within health outcomes, providing a more refined view of the disease state. She noted treatment standards often focus on an average disease profile. But she emphasized that what is really important is the individual patient’s experience and how things are changing over time. Mega sees access to trending patient-generated health data as critical to understanding an individual’s health status.
“I think that the health economics world can really help us quantify the impact that guides and directs this transformation.” — Vivian Lee, MD, PhD, MBA
Mega also credits wearable data with helping researchers understand the diversity within a disease. “If we start to get more input, then we can substratify.” In addition, these data can lead to better treatment decisions. “That’s good for the outcomes of that patient,” she said. “And it’s good for how we essentially pay for healthcare.”
But she also credits these devices with improving patients’ engagement in their care. Even though these tools are often viewed as a one-way data transfer, they are also a way to connect more broadly. She noted clinical trial participants also experienced heightened engagement when outfitted with wearable devices. For example, during the COVID-19 pandemic lockdown, clinical trial participants were often unable to attend in-person visits necessary for clinical study monitoring. “We saw higher participant engagement than we had expected during a pandemic,” Mega said. “People continue to want to stay involved with any assessments they could do remotely.”
Mega added, “I think the idea of bridging what happens in clinics with what happens 365 days out of the year is going to be incredibly powerful, both in research and care.”
Impediments to Acceptance
Despite the tremendous value wearable devices may provide to patients, providers, and payers, wearables still face barriers to acceptance.
These include:
• Accuracy and validity. The absence of clear regulatory oversight policies governing commercial wearable devices has led to the emergence of wearables of unknown safety and efficacy. Inaccurate data may be more harmful than no data.
• Meaningful use criteria and clinical evidence. Few trials have examined the superiority of wearables for clinical outcomes as compared with no wearables.
• Hardware cost and coverage. Cost of wearables may lead to access issues and exacerbate health disparities.
• Data security. Patient-generated health data may be subject to breaches.
• Data management. Challenges with data interoperability.
“These data can lead to better treatment decisions. That’s good for the outcomes of that patient and it’s good for how we essentially pay for healthcare.” — Jessica Mega MD, MPH
How HEOR May Help
Many contributors reiterated the importance of health economics and outcomes research (HEOR) researchers in overcoming these impediments. Albert welcomes HEOR professionals to the wearables world, noting “researchers will be important in validating and verifying the claims made true that the outcomes actually improve.”
Lee concurred, “I think that the health economics world can really help us quantify the impact that guides and directs this transformation.” She added, “We should be challenging digital technology entrepreneurs and innovators to think about how we actually innovate in the payment space to drive these businesses, to deliver services that really improve value for the individual in that way that we talk about in healthcare, and really improve health outcomes and manage reasonable patient expectations.”
Looking Ahead
These products have the potential to change how we deliver and pay for care. But to achieve this goal, HEOR is needed to determine whether these devices truly meet the goals of improving health outcomes, while expanding access and reducing health services utilization.
References
1. MarketsandMarkets. Wearable Technology Market by Product (Wristwear, Headwear, Footwear, Fashion & Jewelry, Bodywear), Type (Smart Textile, Non-Textile), Application (Consumer Electronics, Healthcare, Enterprise & Industrial), and Geography - Global Forecast to 2026. https://www.marketsandmarkets.com/Market-Reports/wearable-electronics-market-983.html. Published April 2021. Accessed August 5, 2021.
2. Phaneuf A. Latest Trends in Medical Monitoring Devices and Wearable Health Technology. https://www.businessinsider.com/wearable-technology-healthcare-medical-devices. Updated January 11, 2021. Accessed August 1, 2021.
3. Pew Research Center. Vogels EA. About One-in-Five Americans Use a Smart Watch or Fitness Tracker. https://www.pewresearch.org/fact-tank/2020/01/09/about-one-in-five-americans-use-a-smart-watch-or-fitness-tracker/. Published January 9, 2020. Accessed August 10, 2021
4. Vailshery LS. Connected Wearable Devices Worldwide. 2016-2022. https://www.statista.com/statistics/487291/global-connected-wearable-devices/. Published January 22, 2021. Accessed August 20, 2021.
5. Aging and Health Technology Watch. The Future of Wearables and Older Adults 2021. https://www.ageinplacetech.com/page/future-wearables-and-older-adults-2021. Published June 2021. Accessed August 1, 2021.
6. Labreck M, Roberts C, Amin A, Sherry M, Sullivan D. B-PO03-003 Cost comparison of outpatient versus inpatient sotalol loading. Heart Rhythm. 2021;18(8):S189-S190. https://doi.org/10.1016/j.hrthm.2021.06.479.