Looking at the Overall Impact of COVID-19 on Healthcare Decision Making
Guest Contributor: Rasika Korde, MSc, PhD, Massachusetts College of Pharmacy and Health Sciences, Boston, MA, USA
Disease burden attributable to the first wave of COVID-19 in China and the effect of timing on the cost-effectiveness of movement restriction policies
Zhao J, Jin H, Li X, et al
Value Health. 2021. 24(5):615-624.
https://doi.org/10.1016/j.jval.2020.12.009
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), also known as coronavirus disease 2019 (COVID-19), has resulted in high morbidity and mortality worldwide. Studies have shown that movement restriction policies (MRPs) like quarantine or isolation for suspected or confirmed cases and travel restrictions for the entire population of the country are effective in delaying or possibly preventing COVID-19 transition. However, MRPs could potentially cause huge productivity losses. Thus, decision makers are unsure whether it is cost-effective to start MRPs early when there are fewer cases and deaths. Different countries have adopted different MRPs and the period between the detection of the first case and the implementation of MRPs has largely varied and the cost-effectiveness of these MRPs is unknown. Within this context, a study by Zhao et al provides insight for decision makers in determining the optimal timing of MRPs for future waves of COVID-19. The study focuses on the first wave of COVID-19 outbreak in China. The authors construct a model that examines the health burden attributable to the first wave of COVID-19 in China and the cost-effectiveness of rapid versus delayed enforcement of MRPs by simulating the potential consequences of MRPs implemented at different time.
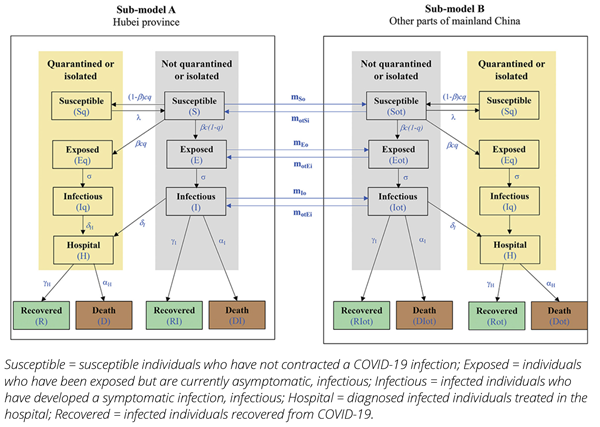
Figure 1. CEA model structure.
Four strategies were compared. Strategy A represents the real-word scenario in China, where the first MRP started on January 23, 2020, and ended on March 25, 2020, when there were no more newly confirmed cases identified in mainland China. Strategies B, C, and D represent a 1-week, 2-week, and 4-week delay in the imposition of MRPs, respectively. For strategies B, C, and D, MRPs end on the day when national newly confirmed cases reach zero. The authors have adopted healthcare as well as societal perspectives, and all costs are expressed in renminbi (RMB; 2019 value) and converted to US dollars using the Organization of Economic Cooperation and Development annual exchange rate for 2019.
The primary outcomes of the study are disability adjusted life-years (DALYs), cost, and net monetary benefit (NMB). Secondary outcomes included the accumulated number of confirmed cases, quarantined/isolated people, and deaths. To capture the initial spread of COVID 19, the model has 2 submodels (Figure 1). Submodel A simulates disease transmission in Hubei province, whereas submodel B simulates disease transmission in other parts of mainland China. Patients who are not quarantined can move between submodel A and B to simulate the disease transmission resulting from population movement between Hubei provinces and other parts of China. Within each submodel, there are 2 modules: one represents individuals who are quarantined or isolated, and another represents individuals who are not quarantined or isolated. On the basis of published epidemiological, disutility, and costing data, the total DALY losses and costs have been calculated for each strategy. The strategy with the highest NMB is considered the most cost-effective. Lastly, to examine the impact of uncertainty, the authors have carried out deterministic and probabilistic sensitivity analyses.
Table 1. Cost and effectiveness results for different strategies.
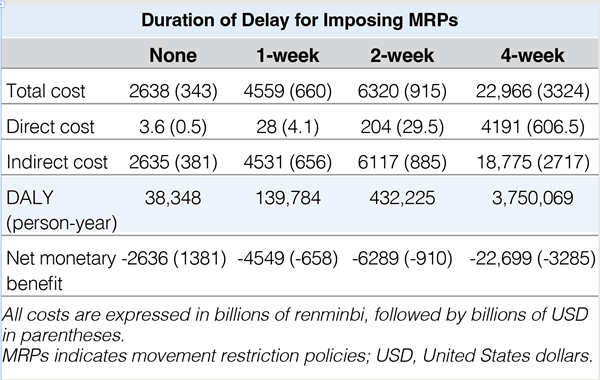
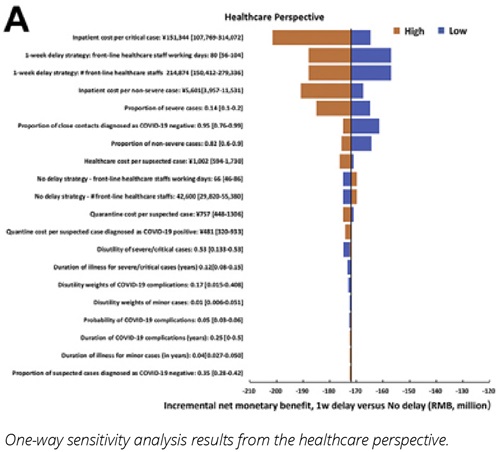
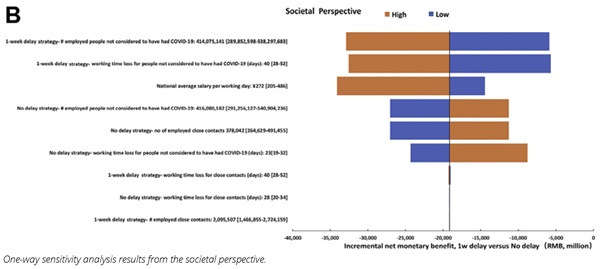
According to the cost-effectiveness analysis (Table 1), strategy A (no delay in MRPs) was the most cost-effective alternative at the willingness to pay of 70,892 RMB, based on healthcare as well as societal perspectives. On conducting a one-way sensitivity analysis from a healthcare perspective, results were most sensitive to inpatient cost per critical case, number of working days for front-line healthcare staff, and number of front-line healthcare staff. From a societal perspective, results were most sensitive to employed people not considered to have had COVID-19, national average salary per working day, and working time lost for people not considered to have had COVID-19 (Figure 2). Results also indicated the number of confirmed cases increased with increasing delay time for MRPs. For example, a 1-week delay in MRPs (strategy B) resulted in 0.463 million confirmed cases versus a 4-week delay (strategy D) resulted in 37.74 million confirmed cases.
Figure 2. Results of one-way sensitivity analyses.
This study supports the findings that early MRPs are more cost-effective than delayed MRPs. This research is highly meaningful as governments have been reluctant to impose MRPs because they pose ethical dilemmas regarding the restriction of civil liberties alongside concerns about the impact on the economy. Quantifying this impact on costs and health of postponement of MRPs reduces uncertainty and supports decision making. One will need to weigh the cost of early implementation of MRPs against the cost of delay to the economy and population health.
This Value in Health article is very timely and useful, as COVID-19 cases in Asian countries (especially China) are on an upward trend again. Plus, as countries across the world are easing travel and social distancing restrictions, there could be a potential surge in COVID-19 cases, which may require decision makers to implement quarantine guidelines all over again. This can be a critical piece of evidence for clinicians, government authorities, and policy makers to plan future pandemic responses and even apply this model to other infectious diseases.