Exploring the Economic and Social Dimension of COVID-19 Vaccination Using a Budget Impact Analysis
Matthäus Traunfellner, MSc; Franz Meyer, BA; Evelyn Walter, PhD, Institute for Pharmaeconomic Research, Vienna, Austria
Background
Since the outbreak of the COVID-19 pandemic in early 2020, more than 500 million infections and more than 6 million deaths have occurred globally.1 To date, the increase in morbidity and mortality associated with COVID-19 has come with enormous financial expenditures for national healthcare systems and societies around the world. Nonpharmaceutical interventions (NPIs), improved diagnostics, and treatment options have mitigated the burden of COVID-19, yet vaccination has proven to be the most effective tool against the spread of the disease.2
However, implementing a successful vaccination campaign incurs high upfront costs for procurement, logistics, and administration of the vaccine, not to mention the intense dedication of medical resources during periods of high viral incidence. Many individuals must be vaccinated within a limited time period to achieve the desired protective effect so that unvaccinated individuals may benefit through herd immunity.3 The emergence of new viral variants with altered immunological and epidemiological characteristics, as well as the decline in vaccine-induced immunity, also necessitate long-term participation of broad segments of the population in a COVID-19 vaccination program. Given the aforementioned efforts, well-suited economic evaluation instruments help policy makers and payers understand the past and future value of COVID-19 vaccination to the general public. Reliable and understandable information obtained in this way can be an important contribution to convincing previously hesitant individuals of the benefits of vaccination. In addition, confidence in vaccination can be reinforced in those who have already been vaccinated, thereby maintaining a willingness to receive booster vaccinations after vaccine-induced immunity has waned. Both effects are important to ensure the sustainable success of the vaccination campaign in the future. In this paper, we analyze the financial and public health impact of COVID-19 vaccination using the Austrian healthcare system and society as examples.
"Nonpharmaceutical interventions, improved diagnostics, and treatment options have mitigated the burden of COVID-19, yet vaccination has proven to be the most effective tool against the spread of the disease."
Our Approach
We performed a budget impact analysis (BIA) to quantify the expected monetary and societal impact of COVID-19 vaccination in Austria. The BIA compares a “world with vaccination” (real-world scenario) to a “world without vaccination” (counterfactual scenario). The model captures the number and costs for hospitalizations, rehabilitation, work absences, and loss of human capital for deceased adult patients in 3 different age categories (18-49 years, 50-64 years, ≥65 years). Vaccination costs are only considered for the vaccination-eligible population in the “world with vaccination” scenario. The time horizon of the model is 2021 to 2023.
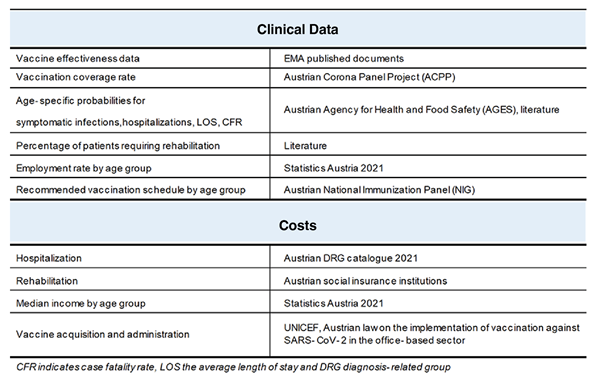
The trajectory of COVID-19 cases, hospitalizations (normal ward, intensive care unit [ICU]), and deaths for the “world with vaccination” and the “world without vaccination” scenario was performed using an online age-structured susceptible-exposed-infectious-removed (SEIR) model for COVID-19 transmission, which was adapted to capture the loss of immunity over time and to model the effects of vaccination.4,5 The SEIR model allows the user to provide inputs on the availability of hospital beds, the effectiveness and availability of used vaccines, the vaccination coverage rate of the adult population, as well as the time-varying reproduction rate RT (Figure 1). The sources of clinical and cost data are provided in Table 1.
Figure 1: COVID-19 Scenario Analysis Tool.*

Table 1: Prevented quarantines and sick leaves.
Results
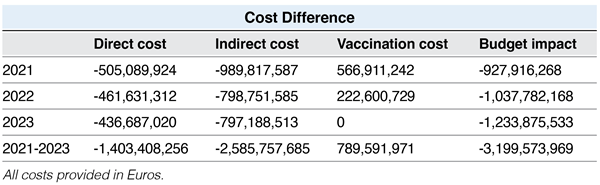
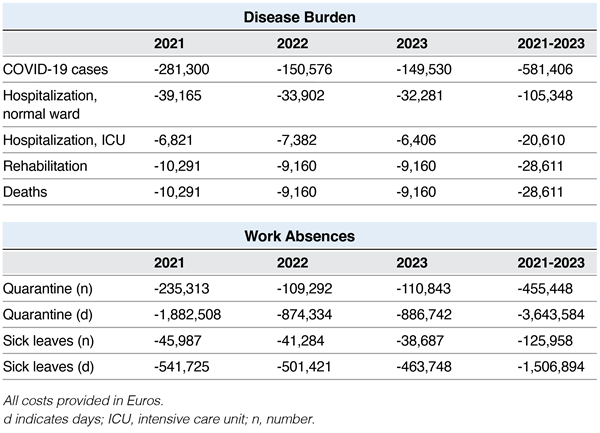
The savings in direct costs, indirect costs, vaccination costs, and the total expected budget impact for the years 2021 to 2023 is shown Table 2. Table 3 summarizes the number of prevented COVID-19 cases, prevented hospitalizations (normal ward and ICU), prevented deaths, prevented quarantines and sick leaves.
"Well-suited economic evaluation instruments help policy makers and payers understand the past and future value of COVID-19 vaccination to the general public."
As shown in Table 2, annual savings in a “world with vaccination” versus a “world without vaccination” range from €927.9 million in 2021 to €1.2 billion in 2023 [total: €3.2 billion]. For direct costs, savings range from €436.7 million in 2023 to €505.1 million in 2021 [total: €1.4 billion]. There are also savings for society. Indirect cost savings range from €797.2 million in 2023 to €989.8 million in 2021 [total: €2.6 billion]. The national health system incurs additional costs for vaccinations ranging from €0 in 2023 to €567.0 million in 2021 [total: €789.6 million].
Table 2: Total budget impact of vaccination in Austria.
The number of COVID-19 cases is lower in a “world with vaccination” versus a “world without vaccination.” 581,406 cases can be averted over the entire observation period. Additionally, 105,348 hospitalizations in the normal ward, 20,610 ICU admissions, 28,611 rehabilitations and 28,611 deaths can be prevented. Finally, 455,448 quarantines and 125,958 sick leaves can be avoided by vaccinating the Austrian population during 2021 to 2023 (Table 3).
Table 3: Prevented COVID-19 cases, hospitalizations, rehabilitations, deaths,
quarantines, and sick leaves in Austria due to vaccination.
Limitations
The present study is associated with certain limitations that must be considered when interpreting the results and applying them to decision-making processes. The model assumes a constant vaccination rate in the adult Austrian population with respect to the first vaccination series and an additional booster vaccination. This assumption is confirmed at the time of the data cut (November 2021) by real-world and representative survey data.6 Lower vaccination rates with booster vaccinations would have a correspondingly lower impact on costs and public health, so future compliance in the population to be vaccinated must be considered. The extent of the long-term consequences of COVID-19 or “long COVID” was difficult to estimate at the time the BIA was drafted; short-term treatment costs for rehabilitation were considered. It is conceivable that additional costs for long-term treatment of patients with long COVID will be incurred in subsequent years. The model does not account for the emergence of new viral variants with altered characteristics of transmission, morbidity, mortality, and vaccine resistance because robust data on the emergence of new viral variants were not available at the time the model was created. In particular, since the emergence of the omicron variant, the incidence, morbidity, and mortality of COVID-19 infections in Austria and worldwide has changed dramatically. Newly developed SEIR models that predict the impact of vaccination in respect of increased vaccine resistance, waning of naturally acquired and vaccine-induced immunity, as well as population exposure to previous virus variants, are now available.7 Revised BIAs incorporating these relevant factors for budget and public health impact of COVID-19 vaccination are areas for further research.
"The number of COVID-19 cases is lower in a “world with vaccination” versus a “world without vaccination.” 581,406 cases can be averted over the entire observation period."
Closing thoughts
Vaccines represent the most important intervention to reduce the likelihood and consequences of COVID-19 infection. Downstream effects of COVID-19 infection such as work absenteeism, hospitalization, rehabilitation, and death can therefore be largely reduced. However, the implementation of successful vaccination campaigns involves high upfront costs for payers and depends on high vaccination coverage in the eligible population. National, regional, and global decision makers, therefore, need transparent and comprehensive tools that are easily adaptable to the dynamic evolution of the pandemic to justify spending on vaccines and to communicate the importance of widespread vaccination programs to the public. Economic evaluation methods such as budget impact analyses are useful tools to accurately assess the value of vaccination to the healthcare system and society as a whole.8
Our results show that the vaccination campaign in Austria has the potential to significantly reduce costs for the healthcare system and society in the period from 2021 to 2023. Savings of €1.4 billion in the healthcare system and €2.6 billion in society are offset by expenditures of €789.6 million for the procurement and administration of vaccines. In addition, 581,406 infections and 28,611 deaths can be prevented between 2021 and 2023.
Although this study is based on an Austrian perspective, we assume that our results are generalizable to European countries with similar healthcare systems, population structure, and vaccination strategy. However, Austrian peculiarities include the exceptionally high testing rate and the relatively low vaccination compliance of the population, especially for booster vaccinations. When transferring our methodology to other country contexts, it is important to use appropriate and recent data on the aforementioned factors. In addition to the Imperial College London model used (no longer updated at the time of this writing), user-friendly models have been developed by the University of Washington Institute for Health Metrics and Evaluation and the Centre for Mathematical Modelling of Infectious Diseases at the London School of Hygiene and Tropical Medicine,9 which have implemented regularly updated country-specific data from low-, middle-, and high-income countries. In addition to the effect of vaccination, these models can also be used to simulate the impact of policy decisions such as travel restrictions, isolation of vulnerable groups, and various testing strategies on pandemic outcomes. Economic models such as budget impact models built on the results of these models then allow the economic and public health impacts of these interventions to be determined. The simplicity and adaptability of the analyses enable continuous adjustment of estimates to dynamic changes in the epidemiologic situation. This is necessary, among other things, when the spread of new COVID-19 variants with altered transmission, morbidity, and mortality parameters; improved pharmacological treatment; or the introduction of new variant-adapted vaccines change the epidemiological situation.
In summary, economic evaluations such as the BIA, which are based on robust and transparent epidemiological models, provide decision makers with reliable and understandable information for the economic and public health value of measures set in the wake of the COVID-19 pandemic. The simplicity and flexibility of the methodology will allow government agencies to rapidly assess the financial and public health implications of adapted vaccination strategies as the epidemiological context changes.
References
1. COVID-19 Dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. John Hopkins University & Medicine, Corona Virus Resource Center. Updated on April 22, 2022. Accessed on April 22, 2022. https://coronavirus.jhu.edu/map.html
2. European Centre for Disease Prevention and Control. Interim guidance on the benefits of full vaccination against COVID-19 for transmission risks and implications for non-pharmaceutical interventions. ECDC; 2021. Accessed on April 22, 2022.
3. Padula WV, Malaviya S, Reid NM, et al. Economic value of vaccines to address the COVID-19 pandemic: a US cost-effectiveness and budget impact analysis. J Med Econ. 2021;24(1):1060-1069.
4. COVID-19 Scenario Analysis Tool. MRC Centre for Global Infections Disease Analysis, Imperial College London. Updated on April 30, 2021. Accessed on June 18, 2021. https://www.covidsim.org/v4.20210430/?place=at
5. Hogan AB, Winskill P, Watson OJ, et al. Within-country age-based prioritisation, global allocation, and public health impact of a vaccine against SARS-CoV-2: a mathematical modelling analysis. Vaccine. 2021;39(22):2995-3006.
6. Panelumfrage zur Corona-Krise. Austrian Corona Panel Project, Universität Wien. Updated on November 5, 2021. Accessed on November 8, 2021. https://viecer.univie.ac.at/coronapanel/
7. Hogan AB, Wu SL, Doohan P, et al. The value of vaccine booster doses to mitigate the global impact of the Omicron SARS-CoV-2 variant. medRxiv. Preprint posted online January 18, 2022. doi:10.1101/2022.01.17.22269222
8. Padula WV, Reid N, Tierce J. Health assessment for COVID-19 treatments and vaccines: will cost-effectiveness analysis serve our needs? Value & Outcomes Spotlight. 2021. January/February:23-25.
9. de Perez EC, Stephens E, van Aalst M, et al. Epidemiological versus meteorological forecasts: best practice for linking models to policymaking. Int J Forecast. 2022;38(2):521-526. The simplicity and flexibility of the methodology will allow government agencies to rapidly assess the financial and public health implications of adapted vaccination strategies as the epidemiological context changes.