Balancing Access and Cost: Innovations Challenge Health Technology Assessment in Asia
Martin Vu, MPH, BSc and Koen Degeling, PhD, MSc, BSc, Cancer Health Services Research, The University of Melbourne, Melbourne, Australia
Funding new high-cost innovations is a challenging policy issue across the Asia Pacific region. As the demand for healthcare in the region continues to grow, several questions have been raised regarding affordable prices, equitable access, appropriate use and availability of innovative drugs, devices, and diagnostics emerging out of clinical development. This session discussed different approaches and opportunities to address these issues across Asia. [Figure 1]
Figure 1. Session speakers (clockwise: Joe Caputo, Marius Van Den Berg; Jeonghoon Ahn; Isao Kamae)
According to session moderator Joe Caputo, BSc (Hons), Vista Health Pte Ltd, Singapore, health technology assessment (HTA) agencies are facing several challenges regarding the evaluation of high-cost innovations. A lack of comparative data on primary endpoints, as well as data availability in general, introduces substantial uncertainty into the decision-making process. The evaluation of medical devices specifically is complicated by the quality of studies and the potential of multiple applications of devices and device-operator interactions that impact effectiveness. For highly innovative technologies, such as CAR-T, it is not always clear whether it is a pharmaceutical or a device, whereas there are often separate processes for each category.
Criteria for Evaluating New Technologies
A new separate evaluation process for innovative technologies has been implemented in South Korea, where technologies need to meet several technical, social, and medical criteria to be eligible. Jeonghoon Ahn, PhD, Ewha Womans University, Seoul, Republic of South Korea, discussed how Korea utilizes internal and external reference pricing, cost-plus pricing, pharmacoeconomic factors, and price-volume agreements to negotiate prices. [Figure 2] Additionally, the country uses 4 different types of risk-sharing agreements, of which contracts based on a refund approach or a maximum budget cap are by far the most often used.
Figure 2. Institutions in the Korean Health Technology Assessment Program.
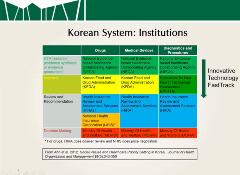
A new system including post-reimbursement evaluations has been proposed in Korea to overcome remaining challenges regarding the effectiveness and cost-effectiveness of high-cost pharmaceuticals after initial listing. This would potentially allow for quicker reimbursement decisions, with the option to re-evaluate the dossier once more evidence on the real-world effectiveness becomes available.
“There is no one-size-fits solution for all, so it is not certain whether the Japanese system is applicable to other countries, but common frameworks in theory can be useful to sustain universal health coverage.”
—Isao Kamae, MD, DrPH
Using ICER to Drive Down Costs
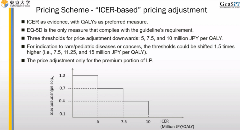
Japan implemented the incremental cost-effectiveness ratio (ICER) into their decision-making process in 2019. Unlike most countries, Japan does not use the ICER for the reimbursement decision, but to adjust the price of drugs with a high budget impact after approval. Isao Kamae, MD, DrPH, The University of Tokyo, Tokyo, Japan, provided an example of how this approach was applied for the use of nivolumab in melanoma, which underwent repricing based on the premiums, sales, and ICER of the pharmaceutical. At its listing in 2014, the unit price of the drug was ¥730,000, which was decreased to ¥365,000 in 2017 and to ¥278,000 in 2018. [Figure 3]
Figure 3. Price adjustment after reimbursement in Japan based on the incremental cost-effectiveness ratio.
Considering the Impact on Patients and Their Families
Marius van den Berg, DBA, Illumina Singapore Pte Ltd, Singapore, highlighted several opportunities to rethink what constitutes value and how it is evaluated through HTA processes. There is great opportunity to move beyond the current reactive HTA processes, where there is a chain of actions and reactions between industry and HTA agencies, to a model where there is a continuous dialogue between these stakeholders. This also relates to the now often siloed parallel processes for pharmaceuticals and devices, which should be harmonized to prevent repetition and promote consistency. Increased consumer participation in HTA is more critical than ever as healthcare is evolving rapidly in a way that not only impacts patients, but also their family members.
“If it wasn’t for the voices of patients, some rare disease diagnoses would not happen and I do believe that the HTA agencies should get more patient organizations involved in these decisions and to listen to the patient side of it and not just always make an economic decision. There are different ways of adding value for the patients.”
—Marius van den Berg, DBA
Adopting Change to Create Accessibility
Despite challenges imposed by high-cost innovations, countries within the Asia-Pacific region have adopted a variety of effective strategies to guarantee equitable access of new medicines and treatment while also maintaining costs. Further opportunities to improve the HTA process in funding high-cost innovations remain. This includes increased consumer engagement, coordination of processes for pharmaceuticals and devices, and post-reimbursement monitoring.