Treatment Journey of Patients With COVID-19 in US Hospital Settings
Rena C. Moon, MD, MPH, Harold Brown, MBA, Ning Rosenthal, MD, MPH, PhD, PINC AI Applied Sciences, Premier Inc, Charlotte, NC, USA
Introduction
While public health measures lowered hospital volume related to COVID-19 after the initial surge in March and April of 2020, the number of COVID-19-related hospital visits was still high throughout 2020.1-4 Furthermore, the number of new cases increased substantially in October 2020 through February 2021, overwhelming the hospital systems again.3,4
Therefore, appropriate allocation of healthcare resources is especially important during the long stretch of a pandemic. To do so, we need a better understanding of the treatment journey of patients with COVID-19—both inpatients and outpatients—including the source of admission, utilizations of intensive care units (ICUs) and invasive mechanical ventilators (IMVs) during their visits.
The main objective of this study is to describe the treatment journey of patients with COVID-19 from the first, or “index” hospital visit to 30 days after discharge for inpatients and hospital-based outpatients in the United States using national real-world data.
Data Source, Study Design, and Population
This study used Premier Healthcare Database (PHD) COVID-19 special release (PHD-SR). PHD-SR is currently being widely used by academic and industrial institutes as well as US government agencies such as the Centers for Disease Control and Prevention and the National Institutes of Health for COVID-19 research.5,6
A retrospective cohort study was performed for all adult (≥18 years old) patients with COVID-19–related visits in the PHD-SR. COVID-19–related inpatient and outpatient visits were identified using the principal or secondary discharge diagnosis of COVID-19 and discharge dates between April 1, 2020 and February 28, 2021. Based on the type of index visit, patients were categorized as either inpatient or outpatient.
Endpoints
Endpoints during an index visit included: point-of-origin (ie, nonhealthcare facility, clinic, transfer from an acute care facility, transfer from a long-term care facility, other), admission through the emergency department (ED) (yes vs no), discharge status (ie, expired, home, home health, transfer to nursing or rehabilitation facility, transfer to another acute care facility, hospice, other), and in-hospital mortality during index visit. For inpatients only, the following endpoints during index hospitalization were also included: ICU admission (yes vs no), IMV use (yes vs no), and extracorporeal membrane oxygenation (ECMO) use (yes vs. no). Endpoints within 30 days after index visit (among patients who did not die during index visit) included: COVID-19-related ED visits, non-ED outpatient visits, hospitalizations (readmissions for inpatients and return hospitalizations for outpatients), hospitalizations with ICU, and inhospital mortality.
"While public health measures lowered hospital volume related to COVID-19 after the initial surge in March and April of 2020, the number of COVID-19-related hospital visits was still high throughout 2020."
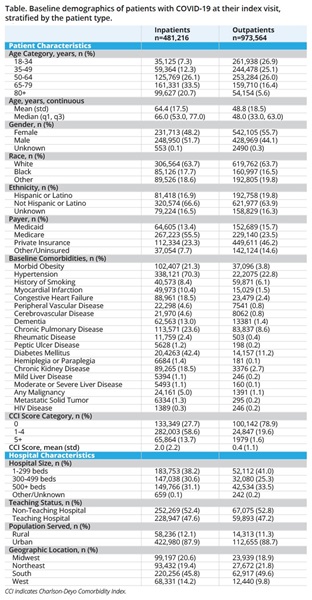
Patient, Visit, and Hospital Characteristics
Patient demographic and clinical characteristics assessed at index visit included age, sex, self-reported race and ethnicity, primary insurance payer, and comorbidities. Hospital characteristics included urban/rural population served, teaching status, US census geographical region (ie, Midwest, Northeast, South,
or West), and size (ie, 1-299, 300-499, 500+ beds).
Comorbidities, including hypertension, history of smoking, morbid obesity, and individual comorbidities in the Charlson-Deyo Comorbidity Index (CCI)7 were identified using discharge diagnosis codes during the index visit or any visit to the same hospital within 180 days prior to the index visit. The CCI score categories (0, 1-4, 5+) were also examined using a previously validated method.8
Statistical Analysis
We used descriptive statistics to present baseline patient, visit, and hospital characteristics of patients with COVID-19 as well as their treatment journey, separately for inpatients and outpatients. All analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, North Carolina, USA).
Results of the Study
A total of 1,454,780 adult patients with one or more COVID-19-related discharges from 909 hospitals were identified in PHD-SR from April 2020 to February 2021. Of these patients, 481,216 (33.1%) were inpatients in 871 hospitals and 983,564 (66.9%) were outpatients in 895 hospitals at their index visit.
Characteristics of COVID-19 Inpatients
Among COVID-19 adult inpatients, the average age was 64.4 years and approximately half were male, about 2/3 were White, 18% were Black, and 17% were Hispanic (Table 1). Comorbidities were common, in the order of hypertension (70.3%), diabetes (42.4%), chronic pulmonary disease (23.6%), morbid obesity (21.3%), chronic kidney disease (18.5%), and congestive heart failure (18.5%). Most patients (45.8%) were hospitalized in the South (reflective of hospitals included in PHD) and in urban hospitals (87.9%), but patients were evenly distributed across small, medium, and large hospitals, categorized by number of beds.
Characteristics of Hospital-Based COVID-19 Outpatients
Among 973,564 COVID-19 adult outpatients, the average age was 48.8 years and 44.1% were male, 63.7% were White, 16.5% were Black, and 19.8% were Hispanic (Table). The most common comorbidities were hypertension (22.8%), diabetes (12.2%), and chronic pulmonary disease (8.6%), but 76.8% of the patients had 0 CCI score. Most patients (53.1%) visited hospitals in the South (reflective of hospitals included in PHD), urban hospitals (79.9%), and small hospitals (1-299 beds, 45.8%).
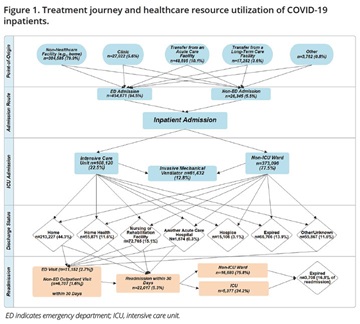
Treatment Journey of COVID-19 Inpatients
Most hospitalized patients originated from a nonhealthcare facility (79.9%) or were transferred from another acute care facility (10.1%), and 94.5% of the patients were admitted through the ED (Figure 1). Of these patients, 22.5% required an ICU stay and 12.8% were put on IMV, and 13.9% died during index hospitalization. Less than half of the patients (44.3%) were discharged home; 15.1% were discharged to a nursing or rehabilitation facility and 11.6% were discharged to home health. After discharge, 2.7% returned to the ED and 5.3% were readmitted to the same hospital within 30 days. Among readmitted patients (n=22,017), 24.2% (n=5377) required ICU admission and 16.8% (n=3708) died.
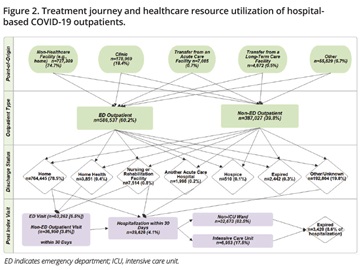
Treatment Journey of Hospital-Based COVID-19 Outpatients
Most outpatients originated from a nonhealthcare facility (74.7%) or clinic (18.4%), and 60.2% of the patients were ED outpatients (Figure 2). Non-ED outpatient visits included diagnostic testing (17.4%), clinic visit only (8.5%), observation (3.8%), and same-day surgery (1.7%). Most patients were discharged home (78.5%) after the index outpatient visit. After discharge, 6.5% returned to the ED and 4.1% had a return hospitalization within 30 days. Among hospitalized patients (n=39,626) within 30 days, 17.5% (n=6953) required ICU admission and 8.6% (n=3420) died during hospitalization.
Closing Thoughts
Our study is the first to report the journey of patients with COVID-19 in US hospital settings using a national database. We would like to note that 95% of inpatients were admitted through the ED. Furthermore, while the percentage of ED utilization was lower (~60%) among hospital-based outpatients compared to that of inpatients, the absolute number of outpatients utilizing ED exceeded that of inpatients (n=454,871 vs n=586,537). Approximately 6% to 7% of outpatients also had follow-up ED visits within 30 days. High utilization of ED among patients with COVID-19 could also hinder the treatment of without COVID-19 ED patients, consequently extending the impact of pandemic to those needing critical care beyond COVID-19.9 Our findings highlight the significant role of EDs during a pandemic and the importance of appropriate resource allocation.
This study also showed high utilization of ICU, IMV, and postdischarge healthcare services among inpatients. Almost a quarter of inpatients were admitted to the ICU and 13% needed IMV use during index hospitalization. A substantial proportion of patients needed continued care either through home health services (12%) or nursing or rehabilitation facilities (15%) or other services (15%) after index hospitalization—indicating a severe burden of COVID-19 on various types of healthcare systems. Our study also showed that in-hospital mortality during index hospitalization was relatively high at 14%.
The proportion of ED utilization was high for both inpatients and hospital-based outpatients in the United States. Among inpatients, the utilization of ICU and IMV were high, and greater than a quarter were discharged to home health or nursing/rehabilitation care facility, highlighting the burden of COVID-19 on various sectors of healthcare services.
References
1. Asch DA, Sheils NE, Islam MN, et al. Variation in US hospital mortality rates for patients admitted with COVID-19 during the first 6 months of the pandemic. JAMA Intern Med. 2021; 181(4):471-478.
2. Nguyen NT, Chinn J, Nahmias J, et al. Outcomes and mortality among adults hospitalized with COVID-19 at US Medical Centers. JAMA Netw Open. 2021;4(3):e210417.
3. The Johns Hopkins University. COVID-19 Dashboard by the Center for Systems Science and Engineering at Johns Hopkins University. Accessed March 26, 2021.
4. Centers for Disease Control. CDC COVID Data Tracker. Centers for Disease Control and Prevention. Accessed March 26, 2021.
5. Lavery AM, Preston LE, Ko JY, et al. Characteristics of hospitalized COVID-19 patients discharged and experiencing same-hospital readmission-United States, March–August 2020. MMWR Morb Mortal Wkly Rep. 2020;69(45):1695-1699.
6. Premier. Premier Healthcare Database Being Used by National Institutes of Health to Evaluate Impact of COVID-19 on Patients Across the US. Published 2020. Accessed March 26, 2021.
7. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-619.
8. Rosenthal N, Cao Z, Chung J, et al. Updated Coding Algorithm for Assessing Charlson Comorbidity Index Using Large Hospital Administrative Data. ISPOR 22nd Annual International Meeting; (PHP184). May 21, 2017; Boston, MA.
9. Gormeli Kurt N, Gunes C. How has COVID-19 pandemic affected crowded emergency services? Int J Clin Pract. 2020;74(12):e13624.
Explore Related HEOR by Topic

