Equitable Prioritization of Health Interventions by Incorporating Financial Risk Protection Weights Into Economic Evaluations
Section Editor: Agnes Benedict; Guest Section Editor: Sugam Mahajan
Hendrix N, Bolongaita S, Villano D, Memirie S, Tolla M, Verguet S. Value Health. 2023;26(3):411-417.
There have been growing concerns about the need to design health policies and decision-making processes that address health equity (ie, who gains and who loses from public health programs). Given a fixed health-expenditure budget, a decision to reimburse a drug for treatment of a disease implies that funds are being diverted from treatments of another disease. Conventional cost-effectiveness analysis (CEA) used around the globe to help decision making rarely informs equity considerations. Frameworks like multicriteria decision analysis, distributional CEA, equity-weighted quality-adjusted life-years, and extended CEA have been developed that can be used by policy makers to ensure equity in distribution of health benefits. However, most of these methods are quite complex and rigorous, as they rely on a social welfare function that is reflective of society’s preferences on inequality that can be difficult to estimate and to comprehend.
Addressing health equity becomes quite relevant in low- and middle-income countries where there is a high incidence of out-of-pocket expenditure on health services, affecting an individual’s ability to seek timely healthcare and be able to afford it. In this context, it becomes important for the policy makers to ensure prevention of medical impoverishment by providing financial risk protection (FRP) to reduce individuals’ risk of excessive out-of-pocket spending on health services via publicly financed health benefits. The authors of this paper published last month in Value in Health set out to develop an analytical framework for incorporating financial risk protection into priority setting for health interventions.
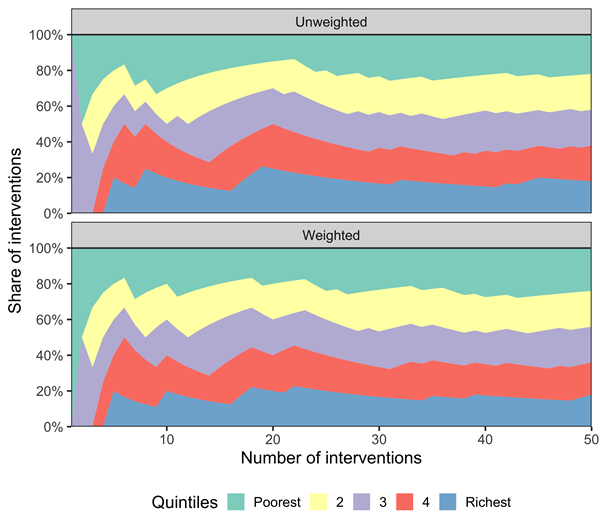
Figure. Proportion of interventions assigned to each income quintile based on rankings of unweighted and weighted deaths averted, as interventions are being selected (according to a decreasing cost-effectiveness) into a publicly financed package of interventions.
The authors identified extended CEA studies reporting health outcomes, costs, and at least one FRP outcome for an intervention (ranging from vaccines, neonatal home care, strengthening surgical units, malaria prevention, among others), with the majority of studies from Ethiopia and India. The common FRP measure was “out-of-pocket expenditures averted” that was converted into ”income-adjusted out-of-pocket averted” by dividing the out-of-pocket expenditure averted by quintile-specific per capita income estimates based on a World Bank Database.
In total, 31 interventions were assessed, including 29 cases reporting out-of-pocket expenditure averted as an FRP metric. FRP weights were estimated based on the distribution of FRP benefits across all interventions considered in the included studies. For each income quintile, the FRP for every intervention was compared in that particular quintile and a higher weight (>1) was given to interventions where the FRP for that particular intervention in that particular quintile was greater than the mean FRP of all interventions in that quintile. Health outcomes (number of deaths averted) were then weighted with the FRP weight.
A league table was then compiled based on unweighted and weighted health benefits and cost-effectiveness by ranking all 145 quintile specific interventions. Using the rankings, an index was created to calculate the probability that a given budget funding N interventions would produce pro-poor distribution (where each quintile received same or higher proportion of interventions compared to richer quintile).
Unweighted rankings produced pro-poor allocations 67% of the time while FRP-weighted rankings were pro-poor 76% of the time. Proportion of interventions assigned to each income quintile based on weighted and unweighted rankings is shown in this figure from the published paper (Figure 3). Unweighted rankings prioritize quintile 3 for first intervention and distribution of interventions was higher for the richer 2 quintiles early on. The weighted rankings produce more equitable distribution.
The framework developed in this study contributes important insights into how health policy makers could prioritize cost- effective interventions to support the economically weaker parts of the society to receive more benefit. Although this approach requires several assumptions (linear scalability of interventions, ability to target specific quintile or quintiles, etc), it focuses on a nonpreference-based risk of illness rather than a social welfare function. Further research is required to see if results and conclusions of this framework would be generalizable.