Polypharmacy and Appropriateness of Prescription Medication Among Community-Dwelling Older Adults
Shaoxi Pan, BS, Hongyan Wu, PhD, School of Public Health, the Key Laboratory of Environmental Pollution Monitoring and Disease Control, Ministry of Education, Guizhou Medical University, Guiyang, China; Beini Lyu, MD, PhD, Institute for Global Health and Development, Peking University, Peking, China
Implications
Polypharmacy and suboptimal use of medication are prevalent among older adults. Interventions such as deprescribing hold promise for addressing these challenges by optimizing medication use. Effective implementation of deprescribing in clinical settings requires the engagement of multiple stakeholders.
Introduction
As the global population ages and the burden of noncommunicable diseases rises, older adults frequently require multiple medications, increasing the risk of polypharmacy. Polypharmacy, typically defined as the simultaneous use of 5 or more medications, is a significant risk factor for adverse drug events. It is linked to increased risk of drug–drug interaction, frailty, impaired cognitive function, and even mortality.1 Addressing unnecessary polypharmacy is crucial for promoting quality of medication use and healthy aging among older adults.
Beyond its impact on health, unnecessary polypharmacy represents a substantial waste of medical resources. It contributes to increased healthcare utilization and costs.2 Estimates suggest that 0.3% of global total health expenditure could be avoided with proper management of polypharmacy.3 In the shift toward value-based care, reducing unnecessary polypharmacy in older adults is essential for delivering cost-effective and beneficial healthcare.
In this recently published study,4 we provided contemporary nationally representative estimates of polypharmacy and appropriateness of medication use among older adults in the United States and identified specific subgroups that are vulnerable to suboptimal medication usage, highlighting the need for interventions.
"In the shift toward value-based care, reducing unnecessary polypharmacy in older adults is essential for delivering cost-effective and beneficial healthcare."
Research Methodology
This study used data from the National Health and Nutrition Examination Survey (NHANES), a comprehensive and nationally representative survey of noninstitutionalized residents in the United States. We analyzed data spanning from the 2011-2012 survey cycle to the 2017-2020 cycle. NHANES collects self-reported data on prescription medication use over the previous 30 days, allowing us to delve into patterns of medication usage, therapeutic classes, and the prevalence of polypharmacy.
Key definitions and metrics were as follow:
- Polypharmacy: the concurrent use of 5 or more medications.
- Hyper polypharmacy: the use of 10 or more medications.
- Potentially inappropriate medication (PIM): assessed based on the 2023 Beers Criteria, which identify medications that pose higher risks than benefits for older adults.
- Appropriate medication use: evaluated against clinical guidelines for heart failure and albuminuria:
- Heart Failure: adherence to American College of Cardiology/American Heart Association guidelines recommending angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs) and beta-blockers.
- Albuminuria: compliance with Kidney Disease Improving Global Outcomes (KDIGO) guidelines recommending ACEIs or ARBs.
Recognizing that patient characteristics may influence both number and appropriateness of medication use, we reexamined the above estimates by subgroups. Subgroups were defined by sociodemographic characteristics (age, sex, race, marital status, education, income, and insurance) and comorbidities (cardiovascular disease, diabetes, chronic kidney disease, and memory problems).
Results
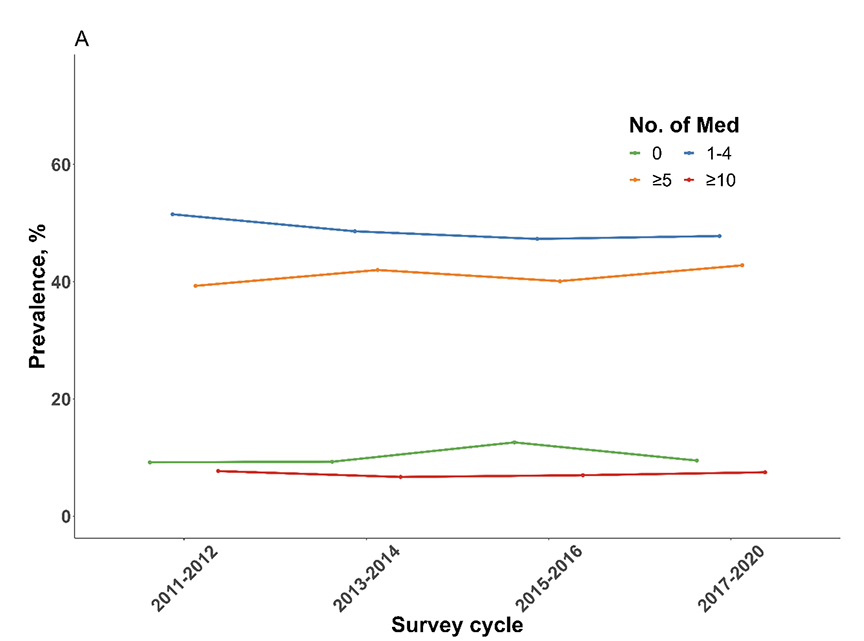
The study analyzed data from a sample of 6336 older adults, with a mean age of 72.9 years, and 55.8% of whom were female. From 2011 to 2020, the mean number of medications used by older adults increased slightly from 4.1 in 2011-2012 to 4.4 in 2017-2020. The prevalence of polypharmacy rose from 39.8% in 2011-2012 to 43.8% in 2017-2020 (Figure 1). Meanwhile, approximately 8% of older adults had hyper polypharmacy. Participants of older age, married or living with a partner, with higher body mass index (BMI), and with comorbidities were more likely to have polypharmacy. Notably, over 60% of older adults with memory problems were affected by polypharmacy.
Figure 1. The prevalence of polypharmacy among community-dwelling older adults in the United States from 2011 to 2020.
In older adults, cardiovascular drugs were the most commonly used medications, with 68.3% using them in 2017-2020. Among these medications, 65.5% used antihypertensive medications. Metabolic drugs were the second most commonly used class, with 52.4% of patients using lipid-lowering medications and 22.7% using glucose-lowering medications. Central nervous system drugs were the third most commonly used category, with 16.3% using analgesics and 13.2% using anticonvulsants.
Potentially inappropriate medication use
The use of at least 1 PIM decreased slightly from 17.0% in 2011-2012 to 14.7% in 2017-2020. PIM use was more prevalent among individuals aged 80 years or above, females, non-Hispanic whites, those with Medicare plus Medicaid, and those with comorbidities. Polypharmacy was associated with higher likelihood of PIM use: 27.0% of older adults with polypharmacy reported PIM, and the most commonly used inappropriately were central nervous system drugs.
Appropriate medication use
For patients with heart failure, only 44.3% used the recommended ACEI/ARBs and beta-blockers. In patients with albuminuria, 54% used recommended ACEI/ARBs. Over the past decade, there has been no significant improvement in the appropriate use of these recommended treatments. Older age, female, living without a partner, having Medicare and Medicaid, and lower income were generally associated with lower likelihood of receiving appropriate medications. Among those with polypharmacy, only 46.8% of patients with heart failure and 67.1% of those with albuminuria received recommended treatment.
Discussion
In this analysis of a nationally representative sample of community-dwelling older adults, we found that the quality of medication use has not improved in the past decade. Issues like polypharmacy and PIM remain prevalent, while the utilization of recommended medications for conditions such as heart failure and albuminuria is alarmingly low. Our results underscore the need to enhance the quality of medication management for older adults and emphasize the urgency for better implementation of targeted interventions to address these ongoing issues.
Our study confirmed that polypharmacy continues to be a common issue among older adults. The complexity of polypharmacy is further compounded when considering the appropriateness of medication use. Our data indicate that many commonly used medications among older adults may be inappropriate, with only a slight reduction in the proportion of individuals using PIMs over the past decade. Alongside of inappropriate medication use, it is crucial to make sure that critical medications with proven clinical benefits are not underprescribed. Our data showed that fewer than 50% of older adults with heart failure and only slightly more than 50% of patients with albuminuria used guideline-recommended medications. Even among patients with polypharmacy, guideline-recommended medications were underprescribed. This underprescription can lead to significant adverse outcomes, such as mortality. The findings suggest that a balanced and comprehensive approach to medication management is needed—one that addresses both the reduction of unnecessary medications and the promotion of essential, beneficial treatments.
One promising strategy to address unnecessary polypharmacy is the practice of deprescribing.5 This approach involves reviewing patients’ medication regimens to taper, stop, discontinue, or withdraw drugs that may no longer be necessary or appropriate. Deprescribing emphasizes patient-centered care and shared decision-making, aiming to manage polypharmacy and improve health outcomes (see Figure 2).
Figure 2. The practice process of deprescribing among community-dwelling older adults
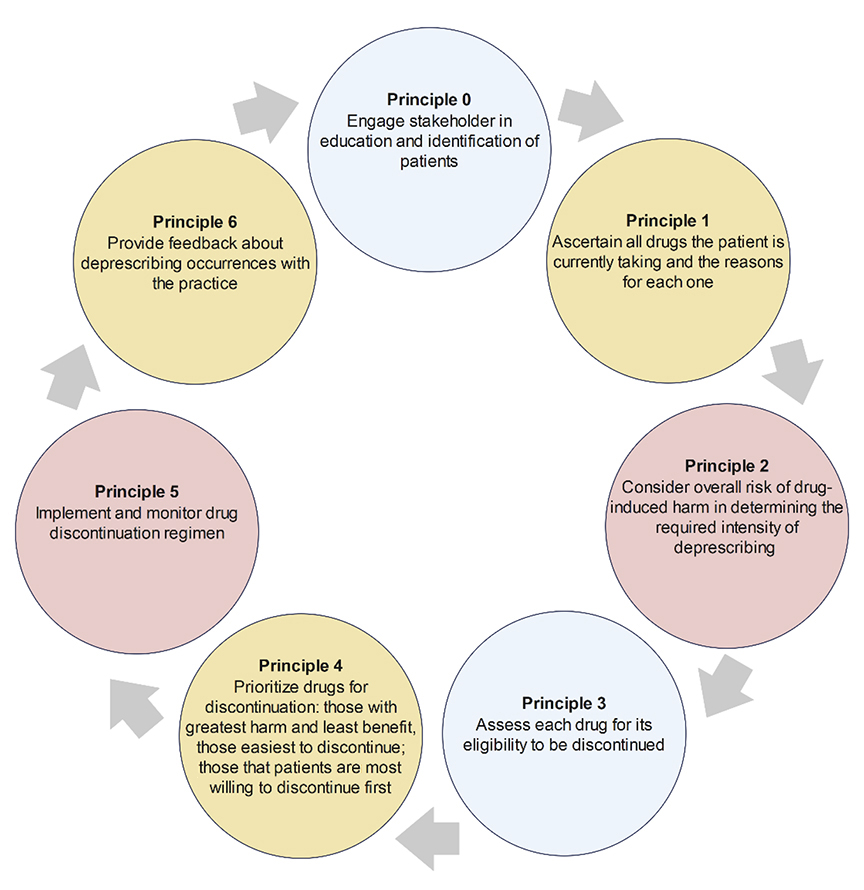
Research supports the benefits of deprescribing, including reduced medication use, decreased PIM prevalence, and improved medication adherence. Additionally, deprescribing can lower medication costs and reduce waste.6 Economic evaluations indicate that deprescribing interventions for community-dwelling older adults are often cost-effective and, in 85% of cases, cost-saving.7 However, the evidence regarding its impact on broader outcomes such as all-cause mortality, fall prevention, hospitalization, and quality of life is less consistent.6
Despite its potential, implementing deprescribing in clinical practice faces significant challenges. Barriers exist at multiple levels—patient, provider, and systemic. The Deprescribing Research Network has developed a socioecological model that categorizes these barriers into individual, interpersonal, organizational, and societal levels.8 Common obstacles include a lack of knowledge and training about deprescribing processes, limited time, fear of adverse consequences, resistance from patients and their caregivers, and the fragmentation of the healthcare system.9 To overcome these barriers, a multidisciplinary and collaborative approach with effective communication is essential.
"Research supports the benefits of deprescribing, including reduced medication use, decreased PIM prevalence, and improved medication adherence."
Conclusion
In summary, our systematic examination of medication use among older adults over the past decade highlights persistent challenges. Polypharmacy, the use of PIMs, and the underutilization of recommended medications continue to be significant issues. Our findings emphasize the need for targeted interventions that engage multiple stakeholders, including healthcare providers, patients, and policymakers, to effectively implement deprescribing and improve the quality of medication management in this vulnerable population.
Disclaimer:
This article is a summarized version of the author’s previously published work and is intended for the readers of Value & Outcomes Spotlight. It does not replace the original publication which is available at: Pan S, Li S, Jiang S, et al. Trends in number and appropriateness of prescription medication utilization among community-dwelling older adults in the US: 2011-2020. J Gerontol A Biol Sci Med Sci. 2024;79(7):glae108. doi: 10.1093/gerona/glae108.
References
- Davies LE, Spiers G, Kingston A, Todd A, Adamson J, Hanratty B. Adverse outcomes of polypharmacy in older people: systematic review of reviews. J Am Med Dir Assoc. 2020;21(2):181-187. doi:10.1016/j.jamda.2019.10.022
- Kwak MJ, Chang M, Chiadika S, et al. Healthcare expenditure associated with polypharmacy in older adults with cardiovascular diseases. Am J Cardiol. 2022;169:156-158. doi:10.1016/j.amjcard.2022.01.012
- Medication safety in polypharmacy. World Health Organization. https://iris.who.int/bitstream/handle/10665/325454/WHO-UHC-SDS-2019.11-eng.pdf?ua=1. Published 2019. Accessed June 9, 2024.
- Pan S, Li S, Jiang S, et al. Trends in number and appropriateness of prescription medication utilization among community-dwelling older adults in the US: 2011-2020. J Gerontol A Biol Sci Med Sci. 2024;79(7):glae108. doi:10.1093/gerona/glae108
- Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175(5):827-834. doi:10.1001/jamainternmed.2015.0324
- Bloomfield HE, Greer N, Linsky AM, et al. Deprescribing for community-dwelling older adults: a systematic review and meta-analysis. J Gen Intern Med. 2020;35(11):3323-3332. doi:10.1007/s11606-020-06089-2
- Sanyal C, Turner JP, Martin P, Tannenbaum C. Cost-effectiveness of pharmacist-led deprescribing of NSAIDs in community-dwelling older adults. J Am Geriatr Soc. 2020;68(5):1090-1097. doi:10.1111/jgs.16388
- Silva Almodóvar A, Keller MS, Lee J, et al. Deprescribing medications among patients with multiple prescribers: a socioecological model. J Am Geriatr Soc. 2024;72(3):660-669. doi:10.1111/jgs.18667
- Robinson M, Mokrzecki S, Mallett AJ. Attitudes and barriers towards deprescribing in older patients experiencing polypharmacy: a narrative review. NPJ Aging. 2024;10(1):6. doi:10.1038/s41514-023-00132-2