Incorporating Patients Into Open-Source Model Development: A Patient-Centered Approach to Health Technology Assessment
Larragem Parsley-Raines, MS, Yuan-Yuan Michelle Cheng, MHS, Richard H. Chapman, PhD, Center for Innovation & Value Research, Alexandria, VA, USA
Introduction: Lack of Patient-Centricity in Traditional Health Technology Assessment
Since the 1960s, health technology assessments (HTAs) have been instrumental in guiding healthcare reimbursement decisions.1 However, HTA has traditionally focused on clinical and economic data, often overlooking the broader needs of patients, caregivers, and other stakeholders directly affected by these outcomes. This exclusion has led to healthcare decisions that often neglect crucial aspects of patients’ quality of life and well-being, resulting in policies that do not adequately address their needs.
In recent years, there has been a push to make HTA more patient-centric. International HTA bodies now require manufacturers to include patient preferences in their HTA submissions for market access and reimbursement purposes. These regulatory changes have set the stage for a more patient-centered approach to HTA. For example, organizations like the European Medicines Agency (EMA) and the National Institute for Health and Care Excellence (NICE) mandate patient involvement, recognizing the value of integrating patient experiences and preferences to ensure comprehensive and relevant assessments.2
The Concept of Patient-Centered Health Technology Assessment
Unlike traditional HTA, patient-centered HTA establishes a meaningful partnership with patients, families, and caregivers throughout the HTA process. This approach emphasizes coleadership and collaboration with decision makers in strategy, governance, and the review and application of results. Patient preferences, outcomes, goal attainment, and lived experiences should be incorporated into HTA methodologies—shaping research questions, designing models, and integrating evidence—to ensure that assessment models and results truly reflect what patients value.
“Learning laboratories” are needed to test innovative, patient-centered approaches to HTA, including testing methods such as multicriteria decision analysis (MCDA) and goal attainment scaling for incorporating multistakeholder perspectives, including patients with lived experience, in building health economic models. The learning laboratory approach aims to establish best practices for patient centered HTA that can be adopted by various healthcare stakeholders through ongoing evaluation and improvement of these methods.
"Patient preferences, outcomes, goal attainment, and lived experiences should be incorporated into HTA methodologies—shaping research questions, designing models, and integrating evidence—to ensure that assessment models and results truly reflect what patients value."
Incorporating Patient Feedback Into Open-Source Models: Role of Patient Stakeholders
Developing open-source models with input from diverse stakeholders is essential for creating transparent and inclusive HTAs. Active participation from patients, caregivers, clinicians, payers, employers, and other stakeholders helps ensure these models reflect real-world complexities. Engaging patients and caregivers captures crucial patient-centered outcomes and experiences, enhancing decision making and ensuring models remain patient-centered. Ultimately, this approach improves health equity by addressing the needs of diverse populations.
Case Study on a Major Depressive Disorder Open-Source Health Economic Model
To employ an inclusive approach in developing our major depressive disorder (MDD) economic model, we convened a multistakeholder advisory group, including over 20 clinicians, health economists, patients, payers, purchasers, and researchers.3
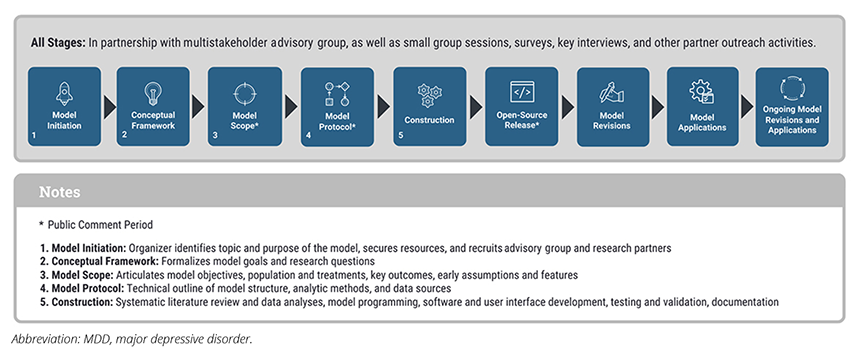
Over the course of 3 years, the multistakeholder advisory group guided the model scope and design, user interface, input parameters, integration of patient priorities and outcomes, and decision contexts. Their input was instrumental in identifying key variables, outcomes, and real-world applications, making the model more relevant to patients and healthcare decision makers. Patients were financially compensated for their time and input and were kept informed as to how their input changed the development of the model (Figure).
Figure. MDD Open-Source Model Development Framework
During the model development, patient feedback provided greater insight into how the MDD open-source model should be designed to be reflective of the patient journey and to capture aspects of patient preferences in MDD treatment modalities that would support healthcare decision making. Patients directly impacted the MDD open-source model in several key areas:
- Changing the model’s focus from treatment-resistant depression to MDD more broadly.
- Adding additional subgroups to include race and ethnicity.
- Including additional cost variables (eg, transportation costs, absenteeism, and presenteeism).
- Designing the user interface to be accessible and user-friendly for technical and nontechnical users, including patients.
- Incorporating treatment gaps to more closely reflect reality, allowing for periods between treatments when patients receive no care.
- Expanding outcome measures beyond traditional metrics (eg, life years, quality-adjusted life years) to include outcomes such as time to first response, number of relapses, etc.
- Modeling relapse as a function of both the degree and timing of the initial treatment response to better mirror real-world experience.
- Including a placeholder for treatment lines, allowing users to input their own data or test hypothetical scenarios.
Patients also expressed the need to address gaps within the MDD open-source model where further research in MDD is warranted, such as including caregiver burden, societal costs, comorbid conditions such as anxiety, diabetes, and cardiovascular disease, and recognizing health equity issues such as access to care and stigma.
Enhancing Patient Partnership in Health Technology Assessment
Patient insights were key to understanding the patient journey, the value of MDD therapies, and the gaps in MDD research that could and should be addressed in the model. Incorporating patients’ feedback was an iterative process, requiring ongoing coordination between patients’ and other stakeholders’ perspectives. In addition, it was challenging to ensure that we were including diverse perspectives that represented the full spectrum of patients with MDD. We also acknowledge that patient inclusion required additional time and resources during the model development process. However, we believe that the final outputs of the MDD model demonstrate the need for patient perspectives in health economic development. The recommendations below emerge out of our work with patients in developing the MDD model.
Meaningful Partnership with Patients
Much remains to be done to ensure meaningful patient partnerships. Tools like the National Health Council’s Fair-Market Value Calculator4 and the Center for Innovation & Value Research’s Blueprint for Patient-Centered Value Research help formalize processes and ensure that no steps are missed. In the case of the MDD open-source model, patients were included in the model development process from the beginning, acknowledged in the dissemination of the research, and compensated for their time and efforts.
"Patient insights were key to understanding the patient journey, the value of major depressive disorder therapies, and the gaps in research that could and should be addressed in the model."
Building Trust With Patient Advocacy Organizations
Ongoing partnerships with patient advocacy organizations are invaluable for HTA. These partnerships aim to strengthen relationships with existing organizations and to engage a broader and more diverse range of patients and patient advocacy groups. For the MDD open-source model, Mental Health America5 was a key partner, supporting efforts including advising on the multistakeholder advisory group, identifying stakeholders such as patients and patient representatives, supporting dissemination efforts of the model, and advocating for the model’s importance for both patients and healthcare decision makers.
Challenges in Identifying and Involving Patients
Unrepresented patients, such as those not affiliated with formal organizations, are often excluded from the HTA process. Challenges in engaging these patients include limited patient networks, communication barriers, and fear of judgment or stigma. Additionally, trust issues may arise when patients feel their voices are not genuinely valued by researchers. When establishing the multistakeholder advisory group for the MDD open-source model, clinicians and patients were the hardest to identify. It was important to cultivate an environment where patients felt safe enough to share their experiences without feeling tokenized.
Importance of Diverse and Representative Patient Involvement
HTA should focus on clinical, financial, quality-of-life, and equity issues. It should reflect diverse patient preferences, goals, and outcomes, and note where patient subgroups are lacking data and implications for decision makers. In the MDD open-source model, patients expressed the need to include inputs that reflected patient subgroups, such as race and ethnicity, adjust for patient heterogeneity, and include additional costing variables.
Need for Understandable and Accessible Explanatory Materials
Most patients and organizations are unfamiliar with HTA. Therefore, it is recommended that accessible explanatory materials be developed, that HTA researchers be trained in patient engagement and communication, and that jargon and specialized terminology be avoided. During the MDD open-source model development process, the multistakeholder advisory group was provided a glossary that included plain language definitions of technical concepts used in the MDD open-source model. During the model-planning sessions, the research team used plain language, thoroughly explained technical aspects of the model, and provided several opportunities for clarification.
Continuous Engagement and Communication
“Closing the loop” on communication fosters active relationships, enabling patients to see how their input is used and its importance in healthcare decision making. Our MDD open-source model development featured continuous engagement during the multistakeholder advisory group meetings, public comment periods, workshops, and dissemination process, which allowed patients to inform and be informed about the HTA process.
References
- Goodman CS. HTA 101: Introduction to Health Technology Assessment. Bethesda, MD: National Library of Medicine (US); 2014.
- Wale JL, Chander D, Collyar D, et al. Can we afford to exclude patients throughout health technology assessment? Front Med Technol. 2021;3:796344.
- MDD Value Model. Center for Innovation & Value Research. https://valueresearch.org/what-we-do/hta-models/major-depressive-disorder/. Published August 13, 2024. Accessed January 24, 2025.
- Access the NHC Patient Compensation Tools. National Health Council. https://nationalhealthcouncil.org/access-the-fmv-calculator/. Published October 8, 2024. Accessed January 24, 2025.
- Mental Health America. https://mhanational.org/. Accessed January 24, 2025.