From the Journals
Section Editor: Agnes Benedict, Executive Director, Thermo Fisher Scientific, PPD Evidera Health Economics & Market Access
Contributor: Paulina Kazmierska, Thermo Fisher Scientific, PPD Evidera Health Economics & Market Access
The Excess Direct Social Costs of Dementia-related Neuropsychiatric Symptoms: A Regionwide Cohort Study Beyond Silos
Zumeta-Olaskoaga L, Ibarrondo O, del Pozo R, Zapiain A, Larrañaga I, Mar J. Value Health. 2025;28(4):536-544.
The behavioral aspects of Alzheimer’s disease are less well-known to the public. These neuropsychiatric symptoms (NPS) include irritability and depression, agitation, apathy, among others—and in the worst cases, motor disturbances, hallucinations, delusions, and disinhibition. These often represent the earliest signs of the disease, posing a source of stress for patients and a substantial challenge for caregivers of dementia patients, which can lead to institutionalization.
In their recent article published in Value in Health’s themed section, The Health Economics of Alzheimer’s Disease and Related Dementias, Zumeta-Olaskoaga et al. aimed to quantify direct nonhealthcare costs disaggregated by the presence of dementia and associated NPS. To this end, the authors performed a retrospective cross-sectional study using electronic health records (EHRs) from health and social care databases of the entire cohort aged 60 and above (n=215,859) in the Gipuzkoa province in Spain.
Given the inadequate coding of NPS in EHRs, the authors used previously developed machine-learning-based algorithms to identify NPS in EHRs based on data on comorbidities and prescribed medications. Direct nonhealthcare costs were defined as the costs of formal services such as residential care centers, day/night care centers, and home help services, as well as cash benefits regardless of their funding (in Spain, part of these costs are financed through copayments, with levels varying by income). Entropy balancing accounted for differences in demographic, clinical, and socioeconomic variables between groups with and without dementia.
The annual costs were calculated based on cash benefits plus product of benefits in natural units each individual received and unit costs. Two-part regression models were used to estimate excess social costs associated with NPS and dementia. The first part estimated the odds of incurring any costs at all (versus none), and the second part used a regression to estimate the mean cost when the cost was higher than zero. Together, the 2 models could be used to estimate average costs for different combinations of covariates. In addition to dementia, NPS, and their interaction, the models included age, sex, Charlson Comorbidity Index, and socioeconomic status.
Among the cohort studied, 3.5% of individuals had dementia, 34.7% had NPS, and 9.6% received dependency benefits. The results showed that dementia and NPS are independently associated with substantially greater odds of incurring direct nonhealthcare costs (odds ratios of 7.36 and 3.23, respectively), but NPS in the presence of dementia does not further increase the odds of incurring such costs.
Both dementia and neuropsychiatric symptoms are also associated with higher social costs, when incurring any (ie, nonzero), and NPS in the presence of dementia leads to additional excess annual costs (ranging from €4161 to €14,929, depending on the reference category). The authors also report that lower socioeconomic status (Figure 1A), higher Charlson Comorbidity Index (Figure 1B), and older age are associated with higher direct nonhealthcare cost.
Figure 1. (A) Mean of the estimated total costs and average of the upper and lower confidence limits of these estimates for each population group by socioeconomic status and (B) Charlson Comorbidity Index.
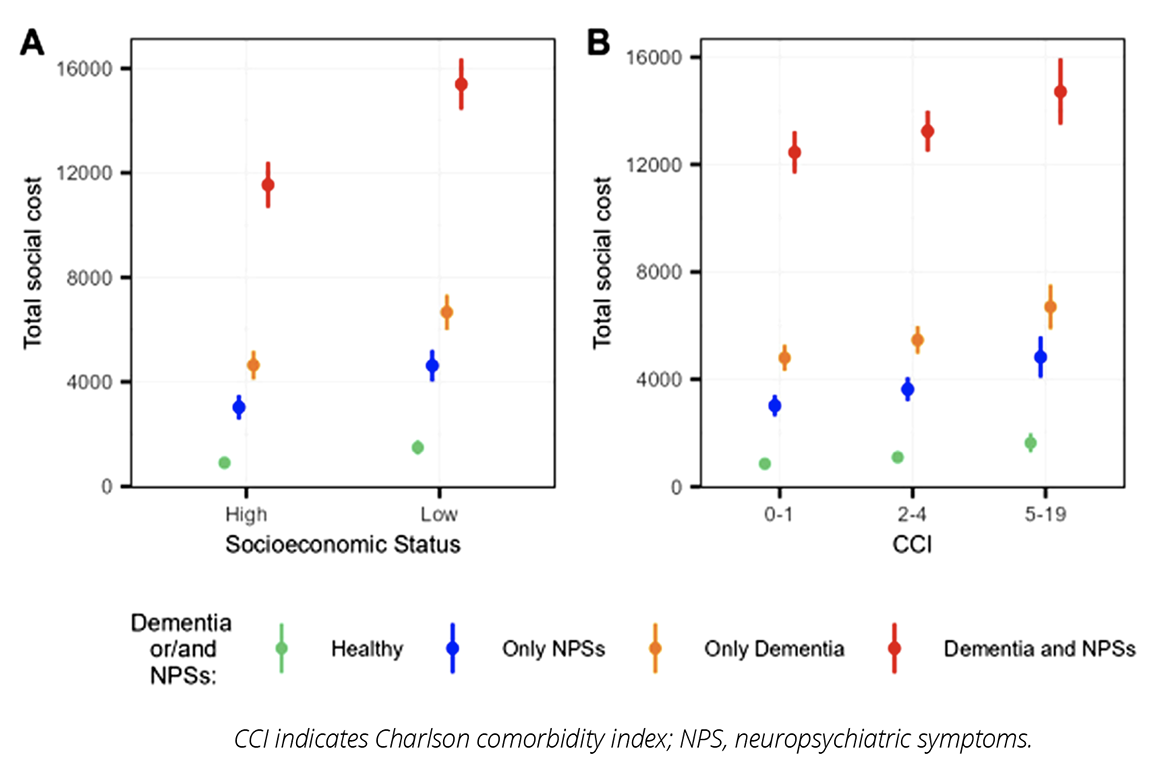
The study provides valuable results as it quantifies the indirect financial impact of dementia and NPS. It highlights how the Spanish long-term care system actually mitigates some of the inequality, since the burden of NPS seems to be greater among patients with low socioeconomic status.
Some limitations apply. The results are specific to the region in which the study was conducted. Cost estimates are not adjusted for the severity of dementia (as EHRs lack this level of granularity of clinical data). Analysis of uncertainty stemming from the use of unit costs would be a valuable addition.
However, study results provide critical inputs to analyses establishing the burden of dementia and NPS and the interventions’ value for money that target dementia and NPS (in Spain, specifically). The study can also serve as a blueprint for similar studies in other jurisdictions.
Editor’s Note: The April 2025 issue of Value in Health featured a special collection of papers on The Health Economics of Alzheimer’s Disease and Related Dementia. The themed section includes an introductory editorial by the Guest Editors, Thomas Rapp and Pei-Jung Lin, and 8 full-length articles. You can read the themed section here.