On Sunday, May 7, 2023 the ISPOR 2023 Patient Representatives Roundtable – North America convened 28 stakeholders representing patient organizations, payers, HTA bodies, government, industry, and researchers and academics to engage various perspectives on the use of Social Determinants of Health (SDOH) data which is a central dialogue point to the current state of healthcare in North America. Targeted discussion centered on key factors that could and should be used to address SDOH including how patient organizations can contribute to the use of SDOH as a tool to improve health equity-relevant data.
Survey on existing viewpoints of patient organizations surrounding Social Determinants of Health (SDOH)
A pre-meeting survey was sent to 37 identified patient organizations to gather current perspectives on and their experience with SDOH. Of the invitations sent, 13 (-35%) individual responses were recorded. A list of detailed results is presented in Appendix 1.
An Overview of Social Determinants of Health
Following the opening of the roundtable and presentation of the survey results from the first roundtable co-chairs, the second co-chair gave a high-level overview of SDOH and how they manifest in the fabric of patient care and advocacy. The various domains of SDOH were highlighted as identified by the Kaiser Family Foundation which includes “Economic Stability,” “Neighborhood and Physical Environment,” “Education,” “Food,” “Community and Social Context,” and “Health Care System.” These domains next manifest into patients’ social needs in how they inform decision-making of basic necessities to the lives of patients. This is weighed against following proper treatment protocols for their disease at all stages of screening, diagnosis, and interventions. The solution to this complete set of scenarios is outside interventions with social needs navigation. The importance of a person-centered care approach is necessary for shaping a good experience through mutual respect, listening, and personal connections between clinicians and patients to promote shared care decision-making and care planning with the goal of joint trust and respect.
Presentation of various stakeholder perspectives regarding the use of Social Determinants of Health (SDOH) data
Three representatives from various stakeholder groups presented their experiences utilizing SDOH within their organizations to promote and improve health equity through SDOH data utilization. Speakers included a patient representative, a payer representative, and a community health center executive.
The first presentation described the viewpoints of a patient representative’s organization’s current projects that are aimed at promoting SDOH data collection with strategies to reach unrepresented patient communities and to broaden understanding of their effects from the scope of Sickle Cell Disease (SCD) populations. The speakers described this hereditary blood disease disproportionately affects black and brown people living within the United States (US) and how a diagnosis of SCD comes with certain stigmas and prejudices. It was reported that only 1 in 4 SCD patients receive the standard of care within the US. SDOH can be highly impactful and increase the burden of managing chronic illnesses. The primary payer for SCD patients in the US is Medicaid whose eligibility requirements are often restrictive and can lead to inadequate coverage for these patients. The organization’s recent works highlight opportunities to improve SDOH data collection by using strategies of strengthening patient engagement, working with trusted community members, addressing stigmas and biases, and using intersectionality as an analytical tool. The organization is working with partners to define disease impacts
and create consensus results using methods that promote a patient-centric design, community engagement, contain multi-stakeholder involvement, and results translated into lay language. Community Health Workers have been utilized with successful results due to their key understanding of culture and socio-economic reality within their communities. The organization is working on a project for an education initiative that will partner with numerous US university leaders on designing curriculums that will lessen bias towards patients with SCD. The final initiative discussed surrounded their Community Health Equity and Research Promotion (CHERP) which will utilize the intersectionality of Patient Reported Outcomes (PROs) using archetypes as communication tools to build and promote empathy.
The second presentation focused on SDOH data from the perspective of a payer organization. This viewpoint demonstrated that SDOH identifies underlying issues outside of clinical care including transportation, home life, and cultural differences for patients. An example was given for patients who must pay for parking in a hospital lot creating a deterrent to walking in the door of a hospital. SDOH is a key component of health equity that cannot be measured accurately and proficiently until SDOH metrics are added for comparison. There is not a current perfect system of identifying and removing bias of data surrounding SDOH nor the incompleteness of current measures, but the current data is better than no data on SDOH at all. Current sources of SDOH data include self-reported responses, provider-reported data, and public data from avenues such as the US census. Areas of concern regarding SDOH data is that many stakeholders, but especially payers, are deterred by the complexity of the data available. Improvement to SDOH data was suggested by following guidelines to keep metrics simplistic, aligned, integrated, and sustainable. Unmet needs have been identified using the Social Inequity Scale which combines core data points and creates prioritized outreach to those areas. Ways of employing SDOH to prevent bias were discussed with the main consideration to remove cost as a primary thought.
The third presentation provided the perspective of a community health center in an urban setting in the US and their programs catering to minority populations that see a high impact from SDOH. The population of attendees of the center are mainly those in the 55-year-old and up community many of whom are African American and are low-income. Health disparities such as race, gender, lower life expectancy, and increased risk for chronic disease also plague this community and commonly bring with them food insecurities, a lack of social inclusion, and a decrease in access to healthcare. The center addresses these factors by providing education and activities that cater to the population. Education programs included fall prevention, self-management resources from evidence-based programs surrounding chronic disease and pain management, and aid in discovering access to benefits and entitlements for health care. Academic partnerships have also been created to improve representation in research and increase trust and health promotion. A detailed list of accomplishments by the center in its long history was provided to document the framework of what a community center’s impact is in addressing SDOH.
Targeted discussion on key considerations for patient organizations and other stakeholders to address and improve SDOH data use.
Non-Adherence in Patients: Non-adherence to treatment can be reported for patients in a multitude of ways though current methods sometimes do not account for SDOH within a patient’s healthcare life cycle. All patients are as adherent as they can be based on their own socioeconomic means and educational understandings. Improvement in the utilization of SDOH regarding reporting patient adherence should be considered with a heavier emphasis for the future.
Improvement is Needed In Collection Methods of SDOH Data: The collection of SDOH data has been ongoing for many years but there is still a need for enhancement in the methods of collecting this data to address gaps and poor setup of collection tools. Progress is also necessary for sharing data between stakeholders rather than employing a proprietary approach.
SDOH Can Affect Different Populations Disproportionately: Though SDOH has a high impact on diverse groups, in the US racism and bias can often disproportionately affect minority populations. There is a greater need to include the potential of systemic problems to improve accountability within the discussion of addressing SDOH. It is difficult to ensure accountability is taking place, but it must be part of the considerations.
Effective Interventions: There is a need to model effective interventions based on a group’s SDOH. Peer support groups and meetings can be an effective tool in the prevention of self-harm for younger individuals who suffer from chronic illnesses that affect their quality of life early on. Stakeholders should be considering how they are shaping interventions to recognize the needs of varied disease groups.
Financial Needs Can Change: In high healthcare utilization groups studies have shown that financial needs are ever changing. A patient can become low-income due to their disease diagnosis and interventions but could also be low-income prior to their interventions. Addressing these concerns may be different and should be approached individually and not a one size fits all approach. Financial queries should be included at multiple stages and not just in initial screenings.
Patient–Centricity Should Be at the Forefront of Addressing SDOH: While including patient-reported outcomes is a norm for the collection of SDOH data, it does not necessarily make the research become patient-centric. Patients should be included in all steps of the process for planning and implantation of research and interventions addressing SDOH.
Research Should Include Disclosures Surrounding SDOH: Many research publications reference SDOH but there is a lack of actual patient participation in discussions. It is recommended that stakeholder groups and publications should look into disclosures on how they have addressed or not addressed SDOH within their research prior to publications.
Social Determinants of Health Are Not Just a United States Problem: Due to the current makeup of the US healthcare system, SDOH has long been considered a US-based concern. Other countries have SDOH problems but due to their makeup such as those with a single-payer system, they can be overlooked by stakeholders due to the bias of healthcare for all leads to access for all.
Conclusions
Social Determinants of Health create a high impact on individuals and the healthcare systems in North America. The topic of SDOH is varied and broad and is not easy to address or improve. Individual factors such as race, education, cultural influences, socioeconomics, and access are all at play in how a patient receives care. An important key consideration for improving SDOH in North America is continued work for organizations and stakeholders to find the right fit to address social needs with an emphasis on a patient-centered model and approach.
Acknowledgments
This summary was developed by Rachel Peoples, MPH. We would like to thank the co-chairs of the ISPOR Patient Representatives Roundtable – North America for their direction and leadership - Alan J. Balch, PhD, Chief Executive Officer of Patient Advocate Foundation and National Patient Advocate Foundation and Lisa J. Pieretti, MBA, Executive Director of International Hyperhidrosis Society. We greatly appreciate all speakers - Ashley Valentine, MRes, Co-Founder and President at Sick Cells; Louis Cabanilla, MSc, Director of Clinical Analytics at Point32Health; and Reneé Cunningham, MSS, Executive Director at Center In The Park, Inc., and all attendees for their participation and valuable contributions.
Appendix 1
Under half of the respondents (-46%) of the pre-meeting survey indicated that their organizations had projects or initiatives focused on understanding or addressing SDOH with the remaining demonstrating either they were not sure of their organization’s SDOH projects or initiatives, or they do not yet have any. While most respondents indicated that their populations served had a significant or above-average social and financial vulnerability level none of the organizations indicated that their populations had a minimal level of vulnerability.
The pre-meeting survey asked organizations to identify how relevant each SDOH domain is to their served populations. The domain determined to be most relevant to participants, with over 90% finding it extremely relevant, was “Health Care Access and Quality.” Many responses represented that “Neighborhood and the Built Environment” were only somewhat relevant. No domain was deemed to be not at all relevant. SDOH was determined to be highly relevant to patient organizations and their leaders view’s represent SDOH has a high impact on their constituents.
Identified patient organizations reported nearly half of the respondents worked with non-rare disease populations versus rare diseases and two organizations self-identified as outside the scope of rare versus non-rare disease advocacy. Specialties identified as the best fit for these patient organizations included Dermatology, Pan Disease, and Neurology. No representatives from Cardiology, Allergy or Immunology, or Oncology were identified as participating in the survey responses.
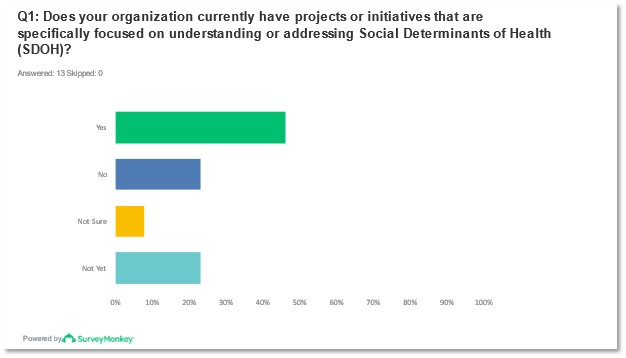
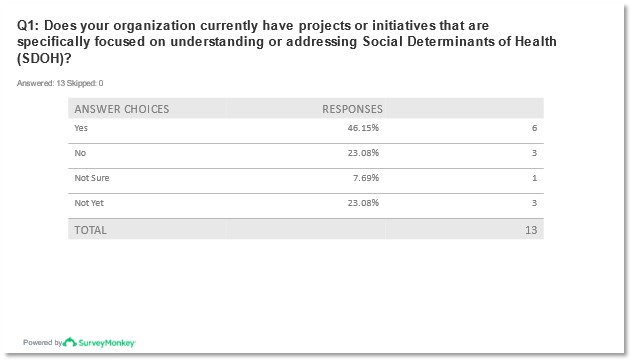
Figures 1 and 2: Reported responses to question 1 from pre-meeting survey.
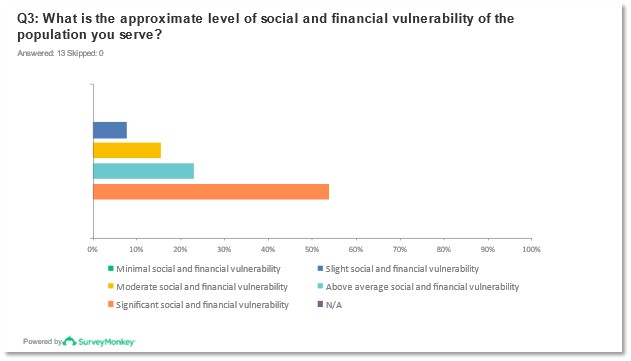
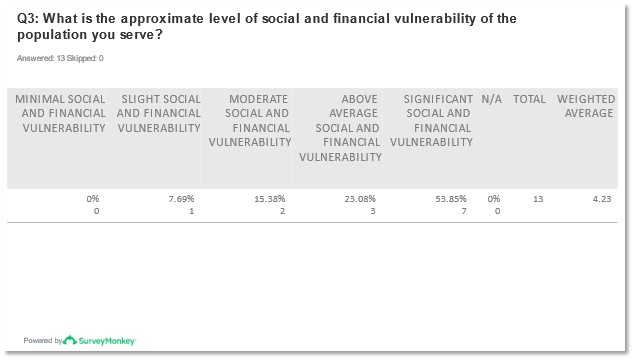
Figures 3 and 4: Reported responses to question 3* from pre-meeting survey.
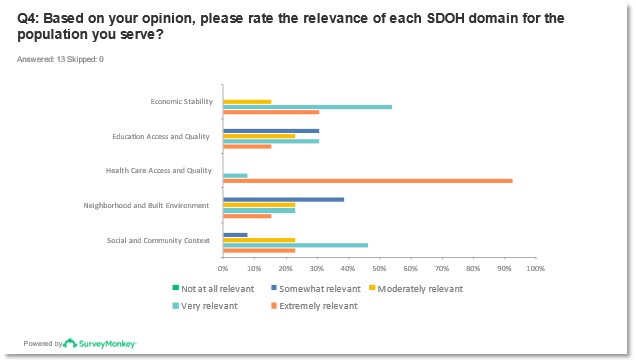
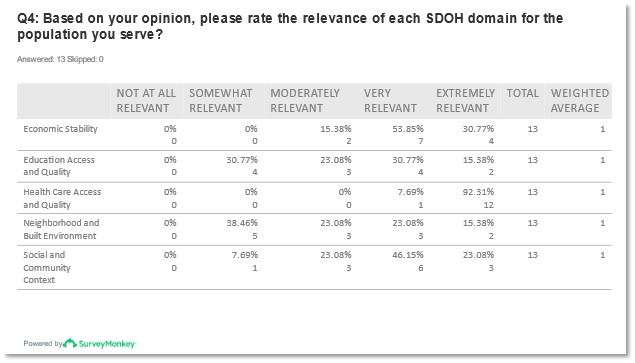
Figures 5 and 6: Reported responses to question 4 from pre-meeting survey.
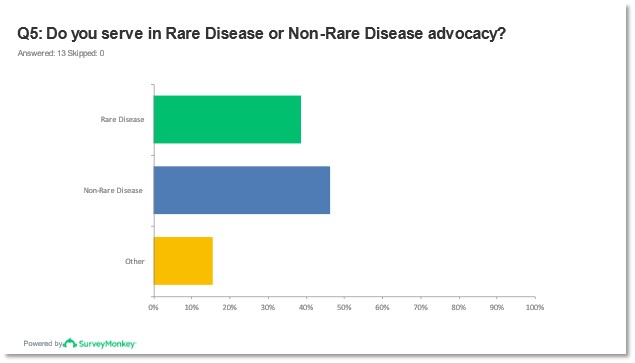
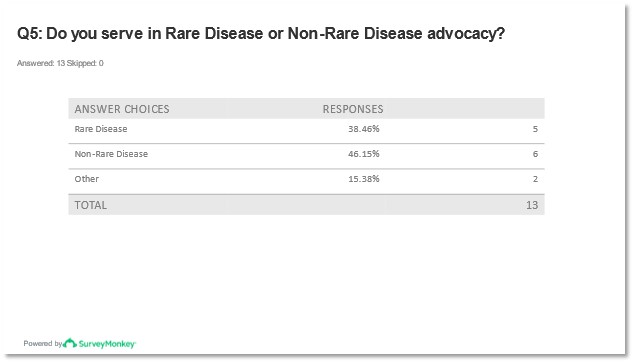
Figures 7 and 8: Report of response to question 5 from pre-meeting survey.
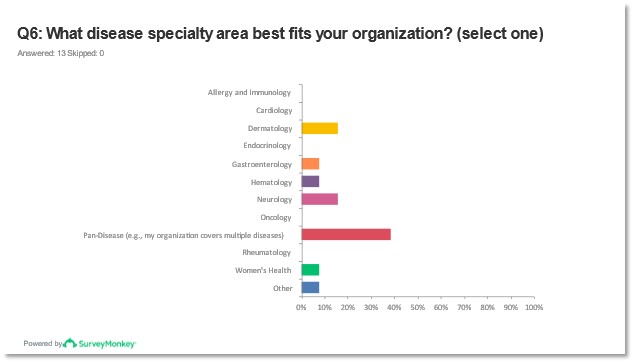
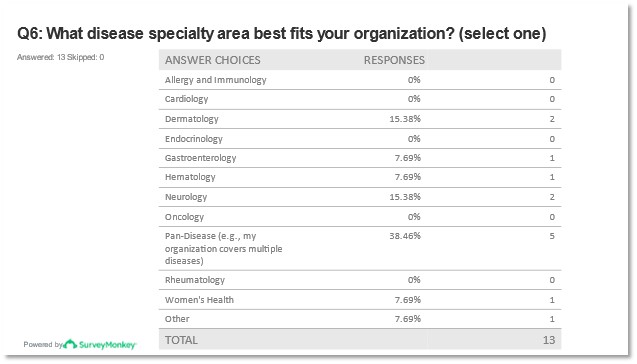
Figures 9 and 10: Report of response to question 6* from pre-meeting survey.
* Questions 2, 7 and 8 of the pre-meeting survey were omitted.