When Increasing Severity of Parkinson’s Disease Leads to Increasing Costs: Results From Register-Based Research in a Swedish Setting
Jenny M. Norlin, PhD, Frida Hjalte, MSc, Klas Kellerborg, MSc, The Swedish Institute for Health Economics, Lund, Sweden; Per Odin, MD, PhD, Skåne University Hospital, Malmö, Sweden; Lund University, Lund, Sweden; SWEPAR-net, Lund, Sweden
Parkinson’s Disease in the Aging Population
Parkinson’s disease is a chronic and progressive neurologic disease that has no cure. With an aging population, the prevalence of Parkinson’s disease is growing, and over the past generation the global burden of Parkinson’s disease has more than doubled.1 Parkinson’s disease is associated with large societal costs2,3 and the disease has a major impact on the health-related quality of life (HRQoL),4 which deteriorates as the disease progresses. The disease is characterized by motor symptoms including shaking, stiffness, and difficulty with walking, balance, and coordination, but also nonmotor symptoms including drooling, constipation, low blood pressure when standing up, voice problems, depression, anxiety, sleep problems, hallucinations, and dementia. In severe stages, people with Parkinson’s disease may have difficulties taking care of themselves and then they require extensive use of formal care such as home help, home healthcare, institutional care, and informal care, that is, unpaid care performed by family and friends.
Few cost-of-illness studies have previously investigated the economic burden of Parkinson’s disease by level of severity of the disease, especially while applying a societal perspective including both direct and indirect costs. In a recently published study5 we analyzed cost and resource use in Parkinson’s disease by severity measured by the Hoehn and Yahr scale, which is a commonly used classification of Parkinson’s disease progression including 5 health states ranging from (1) “Unilateral involvement only usually with minimal or no functional disability” to (5) “Wheelchair bound or bedridden unless aided.” Costs were also presented by percentage of awake time in “off” (“off-time”), which refers to periods of the day when there is poor response to levodopa treatment, causing worsening of Parkinson’s disease symptoms. These severity levels are in line with current health economic modeling practice of interventions in Parkinson’s disease, for which Hoehn & Yahr and “off-time” are the most used health states.
Parkinson’s disease is an illustrative example of a disease associated with aging where a large part of the costs is borne by the municipalities.
Unique Swedish Data
The study was based on the Swedish Parkinson’s disease patient registry, PARKreg. PARKreg has been developed by the Swedish Movement Disorder Society in cooperation with Swedish Neuro Registries since 2012 and includes information on diagnosis, treatments, and outcomes in terms of clinical data and patients’ HRQoL. PARKreg presently includes information on 8200 patients with Parkinson’s disease. The register provides a unique opportunity to analyze real-world data in Swedish clinical practice since observations in PARKreg reflect clinical practice (ie, they occur when patients visit their neurologist and are not protocol driven).
Sweden has a system of unique personal identification numbers that makes it possible to link so-called quality registers, such as PARKreg, to other registries with individual-level administrative data. This creates a unique combination of patient-reported data of HRQoL, physician-reported data of clinical severity, and almost complete administrative data regarding resource use, costs, treatment patterns, and comorbidities.
In our study, we included patients in PARKreg with idiopathic Parkinson’s disease in the Region of Skåne, a relatively large region in southern Sweden, comprising approximately 13% of the total Swedish population. The data were linked to the national prescribed drugs register, which contains close to 100% of all filled prescriptions, and the Skåne Healthcare Register, which contains all healthcare visits to primary care and specialized outpatient and inpatient care.
Patient-reported data on formal care, informal care, transportation, and sick leave were collected from PARKreg. Data on formal care included information on whether the patient stayed at a nursing home, estimates of hours per week with home help or personal assistance, number of visits with home healthcare, and use of an electric wheelchair or electric scooter during the last year.
Data on informal care included number of hours per week that a family member had abstained from work or from leisure time to care for their relative. Information on transportation included the number, type, and length of transportation to healthcare visits during the last year. Patient-reported data on long-term sick leave and early retirement were also collected.
Healthcare contacts included all contacts to primary care, specialized outpatient care, and inpatient care registered with diagnosis codes for Parkinson’s disease. Contacts included visits, inpatient stays, letters, and phone calls as provided by all types of professions such as physicians, nurses, and physiotherapists. All filled prescriptions of antiparkinsonian drugs were included.
With an aging population, the prevalence of Parkinson’s disease is growing and over the past generation, the global burden of Parkinson’s disease has more than doubled.
Parkinson’s Disease and Costs
The overall objective of the study was to estimate resource use and costs, including both direct and indirect costs in relation to levels of disease severity as measured by the Hoehn and Yahr scale and in relation to the periods of the day with poor response to the levodopa treatment (ie, the off-time).
The sample included 1324 observations. The majority (68%) of the observations were reported with Hoehn and Yahr scale stages I and II, 25% with stage III, 6% with stage IV, and 1% with stage V.
This study showed that the more advanced and late stages of Parkinson’s disease are associated with significant societal costs, and a large proportion are costs for formal care. Total mean cost per patient-year was estimated to approximately €16,000 and ranged from about €6000 for Hoehn and Yahr I to €100,000 in Hoehn and Yahr V, as illustrated in Figure 1.
Figure 1. Total mean costs in € 2019 per year according to Hoehn and Yahr stage.
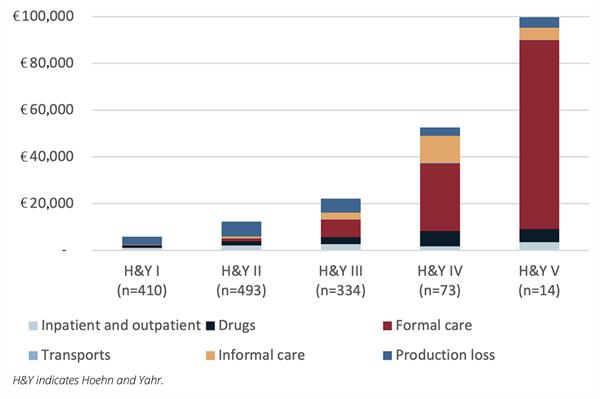
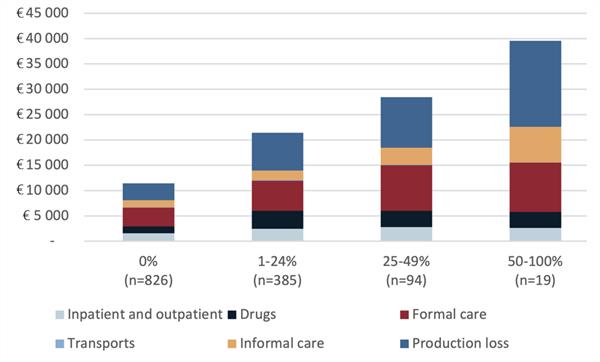
In the early stages of the disease, the dominating part of total costs were indirect costs; accounting for between 50% and 60%. For the more advanced and late stages of the disease, the dominating parts of the costs were formal care, accounting for between 30% and 80% of total costs. The study also demonstrated that total mean costs increased with increasing off-time (Figure 2).
Figure 2. Total mean costs in € 2019 per year according to “off-time.”
The Problem of Budget Silos
As our study shows, Parkinson’s disease is an illustrative example of a disease associated with aging where a large part of the costs is borne by the municipalities. Because healthcare in Sweden is provided by the regions, these different cost-bearing silos may cause poor economic incentives to provide cost-effective care for this patient population. For example, device-aided therapies for Parkinson’s disease, which include deep brain stimulation (surgical insertion of treatment electrodes in the brain) and pump-based continuous delivery of levodopa-carbidopa intestinal gel, levodopa-entacapone-carbidopa intestinal gel, or apomorphine to avoid motor fluctuations and dyskinesias (unwanted movement), have shown to be difficult to implement in clinical practice even though they are considered cost-effective therapies.7 This could be caused partly by the fact that the relatively high costs of providing device-aided therapies are borne by the regions, whereas the benefits, in terms of large cost offsets due to reduced need for home help and nursing homes, are captured mainly by the municipalities. The problem is that budget silos (which has been discussed elsewhere8-10) will become increasingly challenging with an aging population and with an increased prevalence of aging diseases such as Parkinson’s disease.
Parkinson’s disease is an illustrative example of a disease associated with aging where a large part of the costs is borne by the municipalities.
Closing Thoughts
In conclusion, our study shows that Parkinson’s disease is associated with significant societal costs, which increase considerably as patients in advanced and late stages often require resource-intensive and costly formal care. Consequently, substantial cost savings can potentially be made by optimizing the healthcare of patients in advanced and late stages, and by putative future disease-modifying therapies.
As future putative disease-modifying therapies become available for people with Parkinson’s disease, the industry, healthcare providers, and payers need to overcome challenges including budget silos and affordability to ensure sustainable and timely access to these therapies.
References
1. GBD 2016 Parkinson’s Disease Collaborators. Global, regional, and national burden of Parkinson’s disease, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17(11):939-953.
2. Findley LJ, Wood E, Lowin J, Roeder C, Bergman A, Schifflers M. The economic burden of advanced Parkinson’s disease: an analysis of a UK patient dataset. J Med Econ. 2011;14(1): 130-139.
3. von Campenhausen S, Winter Y, Rodrigues e Silva A, et al. Costs of illness and care in Parkinson’s disease: an evaluation in six countries. Eur Neuropsychopharmacol. 2011:21(2):180-191.
4. Norlin JM, Kellerborg K, Odin P. Patient utilities in health states based on Hoehn and Yahr and off-Time in Parkinson’s disease: a Swedish register-based study in 1823 observations. Pharmacoeconomics. 2021. Online ahead of print.
5. Hjalte F, Norlin JM, Kellerborg K, Odin P. Parkinson’s disease in Sweden-resource use and costs by severity. Acta Neurol Scand. 2021. Online ahead of print.
6. Hoehn MM, Yahr MD, Parkinsonism: onset, progression and mortality. Neurology. 1967; 17(5):427-442.
7. Norlin JM, Willis M, Persson U, Andersson E, Pålhagen SV, Odin P. Swedish guidelines for device-aided therapies in Parkinson’s disease-Economic evaluation and implementation. Acta Neurol Scand. 2021:144(2);170-178.
8. Drummond M, Jonsson B. Moving beyond the drug budget silo mentality in Europe. Value Health, 2003:6(suppl)1:S74-S77.
9. Garrison L, Towse A. The drug budget silo mentality in Europe: an overview. Value Health. 2003;6(suppl)1:S1-S9.
10. Gozzo L, Benfatto G, Giorgianni F, et al. Beyond the budget silo approach: estimating health system sustainability for future dementia drugs. Pharmadvances. 2020;2(3):68-78.