Medication Management Practices for Noncommunicable Diseases During the COVID-19 Pandemic: A Snapshot of the European Situation
Tamás Ágh, PhD, Syreon Research Institute, Budapest, Hungary; Job FM van Boven, PhD, University of Groningen, Groningen, The Netherlands; Björn Wettermark, PhD, Uppsala University, Uppsala, Sweden and Vilnius University, Vilnius, Lithuania; Enrica Menditto, PhD, University of Naples Federico II, Naples, Italy; Hilary Pinnock, PhD, University of Edinburgh, Edinburgh, Scotland, England, United Kingdom; Ioanna Tsiligianni, PhD, University of Crete, Crete, Greece; Przemyslaw Kardas, PhD, Medical University of Lodz, Lodz, Poland, on behalf of the European Network to Advance Best Practices & Technology on Medication Adherence (ENABLE)
Introduction
The appropriate management of noncommunicable diseases (NCDs) is important during a pandemic; however, the intensive focus on COVID-19 prevention, the management of patients with COVID-19, and the lockdown and physical distancing restrictions adversely affected NCD-related healthcare services.1 In May 2020, the World Health Organization surveyed service delivery for NCDs across 155 countries and found that in 75% of countries around the world there was considerable disruption to NCD services due to COVID-19.1 Across services, rehabilitation was the most impacted, with 79% of countries in Europe reporting disruption to rehabilitation services.1
The continuity of medication therapy is a cornerstone for the effective management of NCDs.2 Even before the COVID-19 pandemic, about 50% of people with NCDs were nonadherent to their medication,3 which can have potentially serious negative consequences on their health outcomes (eg, increased risk for cardiovascular events).4 Continuous access to medication is a prerequisite for appropriate treatment adherence, which disruptions of healthcare services may compromise due to COVID-19.
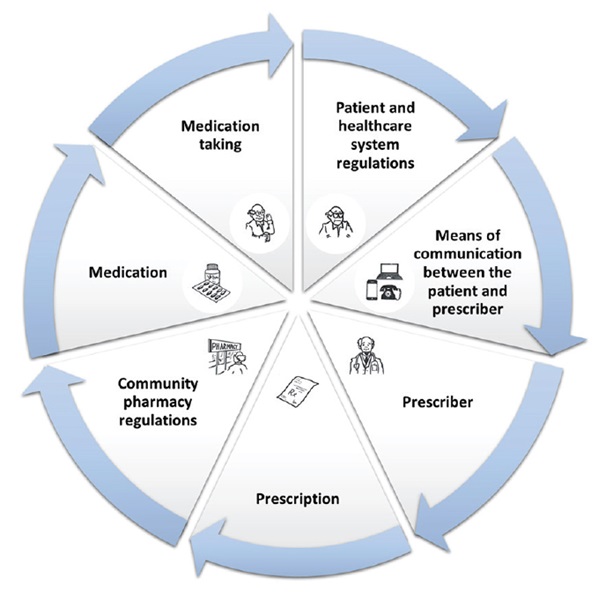
The European Network to Advance Best Practices & Technology on Medication Adherence (ENABLE; CA19132), launched in October 2020, is a 4-year research initiative funded by the European Commission under the COST Action program.5 Among others, ENABLE aims to evaluate current practices related to medication management (Figure 1). Given increasing concerns that patients with NCDs may not be receiving appropriate care or access to their medication during the COVID-19 pandemic1, ENABLE considered it important to assess the medication management practices in place for NCDs during the COVID-19 pandemic across European countries and to evaluate its association with the population burden of COVID-19 and country income.
Figure 1. Medication management cycle
Survey on medication management practices during the COVID-19 pandemic
In December 2020, ENABLE conducted a cross-sectional, web-based survey in 38 European countries and Israel on available medication management services for NCDs. A 33-item, English language questionnaire was developed based upon 7 domains of the NCDs medication management cycle defined by ENABLE working group (Figure 1).
Descriptive statistics, non-parametric tests, and generalized linear models were applied to analyze the data. The population burden of COVID-19 was defined in line with the European Centre for Disease Prevention and Control as the number of COVID-19 cases and COVID-19 deaths per 100,000 inhabitants6 and country income was assessed as gross domestic product per capita (GDP/capita) at purchasing power parity.7 This survey was reported according to the Checklist for Reporting Results of Internet E-Surveys (CHERRIES).8 A more detailed description of the methodology is described elsewhere.9
Continuous access to medication is a prerequisite for appropriate treatment adherence, which disruptions of healthcare services may compromise due to COVID-19.
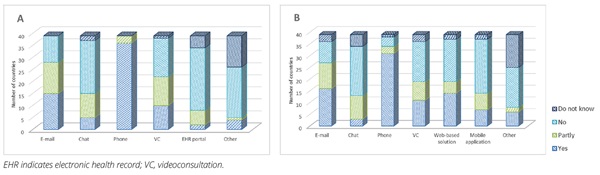
From the 92 invited ENABLE collaborators, 53 experts (ie, healthcare providers and academics with medical or pharmaceutical backgrounds) from all 39 target countries completed the survey. In 35 (90%) of the evaluated countries, there were disruptions to face-to-face consultations in primary care and/or outpatient clinics due to the COVID-19 pandemic. Disruption to face-to-face healthcare services showed a positive association with the number of COVID-19 cases (mean±SD in countries with “yes,” “partly,” and “no” disruption: 3655.1±1561.9, 4580.4±1818.9, and 1772.9±712.5; p=0.03) and a positive trend with the number of COVID-19 deaths (mean±SD in countries with “yes,” “partly,” and “no” disruption: 73.2±41.9, 82±37.7, and 23±17; P=.05 per 100,000 inhabitants. In the evaluated 39 countries, the mean±SD number of available e-health services for symptom monitoring and patient management (eg, e-mail, online chat, phone, videoconference, electronic health record portal, or other) and teleconsultation methods for requesting prescriptions for chronic medications (eg, e-mail, online chat, phone, videoconference, web-based solution, mobile application, or other) was 3±1.3 and 3.4±1.6, respectively. The mean±SD number of available e-health services for the management of NCDs showed a trend to be lower in upper/middle (2.1±1.1) compared to high income countries (3.2±1.3; P=.05). In contrast, the number of available teleconsultation methods for requesting prescriptions did not correlate with country income (upper/middle income countries: 2.9±1.6 versus high income countries: 3.5±1.6). The available forms of e-health services and options for requesting medication prescriptions were different across European countries. In most countries, phone and e-mail were the most commonly available modes of teleconsultations between patients and physicians during the pandemic in December 2020 (Figure 2). However, in countries with higher GDP per capita, a more comprehensive range of e-health services (eg, online chat, video consultations, communication via the electronic health record portal, alerts when prescriptions need to be renewed, online ordering of prescription medication) were available for patients with NCDs.
Figure 2. Availability of various forms of e-health services for symptom monitoring and patient management (A), and teleconsultation modalities for requesting chronic medication prescriptions (B)
Our survey highlights differences in the availability of face-to-face services and the number of e-health services during the pandemic across European countries. Further large-scale studies are warranted to better understand the long-term clinical and economic consequences of the considerable disruption of face-to-face NCD services due to COVID-19 and to validate the trends observed in this study (ie, the association between the disruption to face-to-face healthcare services and the number of COVID-19 deaths per 100,000 inhabitants and between the number of available e-health services for the management of NCDs and country income).
Disparities in the availability of face-to-face services and the number of e-health services in the management of patients with NCDs points to the need for a paradigm shift to optimize access to healthcare services and treatments during the COVID-19 pandemic and beyond.
Based on our findings, several practical solutions could be suggested to ensure access to NCD treatments during the pandemic, including:
• an increased range of remote services for ordering repeat prescriptions (eg, online, via mobile app),
• expanding the scope of professionals authorized to prescribe medications (or issue repeat prescriptions) via e-health services,
• increasing the duration of prescriptions (although this needs to be balanced with managing shortages and whether appropriate given the medication and the disease),
• allowing substitution of unavailable drugs (should consider existing comorbidities and comedication),
• creating e-health systems supporting patients in long-term treatment, encouraging patient empowerment and patient-centered care, and
• providing publicly available guidance on strategies for maintaining treatment during the pandemic lockdown.10
Our results should be considered in light of certain limitations. The self-developed questionnaire and multiple-choice questions with closed answers allowed us to seek precise information; however, it may be biased as the questionnaire was available only in English and was not translated to the native language of the participants. The survey was conducted among ENABLE collaborators whose views represent one perspective only and cannot be considered representative. It is also important to highlight that in this survey only the availability of healthcare services was assessed, but data on healthcare resource utilization were not collected. Finally, this survey represents the situation in December 2020, and findings may have differed substantially if the survey had been distributed at another time.
Conclusions
The COVID-19 pandemic limited the number of face-to-face appointments in patient care; however, e-health modalities for managing NCD patients were available in many European countries. Disruption to face-to-face consultations was associated with a greater population burden of COVID-19 and the number of available e-health services was associated with higher country income. Disparities in the availability of face-to-face services and the number of e-health services in the management of patients with NCDs points to the need for a paradigm shift to optimize access to healthcare services and treatments during the COVID-19 pandemic and beyond.
References
1. World Health Organization. The impact of the COVID-19 pandemic on noncommunicable disease resources and services: results of a rapid assessment. Geneva: World Health Organization. 2020.
2. Kluge HHP, Wickramasinghe K, Rippin HL, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet. 2020;395(10238):1678-1680.
3. World Health Organization. Adherence to long-term therapies: evidence for action. Geneva: World Health Organization. 2003.
4. Chowdhury R, Khan H, Heydon E, et al. Adherence to cardiovascular therapy: a meta-analysis of prevalence and clinical consequences. Eur Heart J. 2013; 34(38):2940-2948.
5. van Boven JF, Tsiligianni I, Potočnjak I, et al. European Network to Advance Best Practices and Technology on Medication Adherence: Mission Statement. Front Pharmacol. 2021;12: 748702.
6. European Centre for Disease Prevention and Control. Situation Updates on COVID-19. Accessed March 7, 2021. https://www.ecdc.europa.eu/en/covid-19/situation-updates
7. World Bank. GDP Per Capita at PPP in Current International USD. Accessed January 07, 2021. https://data.worldbank.org
8. Eysenbach G. Improving the quality of web surveys: the checklist for reporting results of internet e-surveys (CHERRIES). J Med Internet Res. 2004;6(3):e34.
9. Ágh T, van Boven JF, Wettermark B, et al. A cross-sectional survey on medication management practices for noncommunicable diseases in Europe during the second wave of the COVID-19 pandemic. Front Pharmacol. 2021;12:685696.
10. Kardas P, van Boven JFM, Pinnock H, et al. Disparities in European healthcare system approaches to maintaining continuity of medication for noncommunicable diseases during the COVID-19 outbreak. Lancet Reg Health Eur. 2021;4:100099.

