Characterizing the Occurrence of Stroke in Long COVID: How Can We Assess This Evolving Topic?
Charlotte Fleming, MSc, Prerna Patel, MSc, MPH, Clarivate, Oxford, England, United Kingdom; Angsheeta Chakraborty, PharmD, Clarivate, Bangalore, India; Tara Jaiswal, MPharm, Clarivate, Gurgaon, India; and Sunita Nair, PhD, PGDip, Clarivate, Mumbai, India
The past 2 years of public health surveillance have shown that complications from SARS-CoV-2 infection are not limited to the respiratory system, with some patients presenting with cerebrovascular disease and stroke.1,2 Available data indicate that most patients hospitalized due to severe COVID-19 infection consequently have other neurological complaints related to the brain or nervous system. A severe infection increases the risk of vascular damage and cerebrovascular complications, which are more likely to occur in patients who were critically ill and hospitalized.1
Postacute COVID-19 syndrome, known as ‘’long COVID,” describes lingering complications that extend ≥4 weeks beyond the initial symptoms of COVID-19.2 This is an evolving topic of interest for the health economics and outcomes research (HEOR) community, as it impacts health policy and strains health resources.3 Despite 2 years’ worth of published biomedical literature from the COVID-19 pandemic at our disposal, there is a paucity of evidence that assesses the relationship between long COVID and the onset of stroke, particularly in patients in recovery from critical care. Stroke is often reported as a major adverse cardiovascular event; however, it was classified as a neurological disease in 2017,4 and thus may be categorized as a neurological complication in long COVID.
Our review identified multiple confounders that impacted our ability to assess the relationship between long COVID and the onset of stroke.
A systematic literature review is an essential component in evidence-based practice and ensures that all outcomes of interest are pooled and appraised to answer a research question. We conducted this systematic literature review to identify studies reporting stroke-related outcomes in patients suffering from long COVID who were previously hospitalized for a severe COVID-19 infection to assess how these outcomes have been reported and whether there is an increased risk of stroke in this patient group.
The systematic literature review was performed in accordance with the Cochrane and PRISMA guidelines and consolidated the findings of relevant peer-reviewed research published between January 2020–June 2021 into a conference proceeding for an ISPOR conference, which was published in Value in Health.5 The review was subsequently updated in January 2022 for this Value & Outcomes Spotlight article. Biomedical literature databases, among other sources (eg, conference proceedings from stroke journals, COVID-19–related guidelines and web sources, active/recruiting clinical trials) were searched.
Studies reporting patients with long COVID (ie, diagnosed ≥4 weeks after initial infection and discharged from critical care), were appraised with no restriction by country/region. Outcomes including secondary cerebrovascular events and stroke characteristics were of interest.
Large-scale studies on long COVID rarely include stroke-related outcomes
Of the 5628 publications that were assessed in the systematic literature review, a total of 4 published studies (2 medical chart reviews and 2 prospective observational studies) and 4 ongoing clinical trials were found relevant in the original 2021 review. An additional 3 retrospective cohort studies and 2 interventional trials were identified in the 2022 update. Studies were conducted in Europe, India, Iran, Ukraine, and the United States, and measured a range of stroke-related outcomes from the onset of long COVID up to 92 days’ follow-up. The study designs, along with the reporting of cerebrovascular events and neurological complaints, were variable. Therefore, the evidence was not suitable for quantitative analysis. The incidence of stroke post-discharge ranged from 0.45% (United States) to 11.5% (Ukraine). The onset of thrombosis occurring after hospital discharge ranged from 1.61% to 2.5% in the United States, with only 1 study reporting arterial thromboembolism (0.7%). A single study reported the mortality due to stroke at 0.59% (Iran) and another study measured a composite outcome of cerebrovascular events.
Overall, our review identified a dearth of peer-reviewed literature that had measured stroke-related outcomes at timepoints associated with long COVID. We found clear discrepancies in the definition of long COVID, for example, in studies measuring stroke-related outcomes <4 weeks from a severe COVID-19 infection. This timepoint is in contrast to the World Health Organization’s definition of long COVID (ie, complications extending ≥4 weeks beyond initial symptoms)6 that we adopted as an inclusion criterion. Consequently, much of the literature was deemed ineligible during the review process.
A deeper understanding of the postacute COVID-19 pathogenesis and a wider, more homogenous evidence base are required to assess whether there is any clinically significant relationship between long COVID and stroke.
The identification of evidence gaps by a rigorous systematic literature review process can influence the practice of evidence-based medicine and drive decision making. Our review identified multiple confounders that impacted our ability to assess the relationship between long COVID and the onset of stroke, including anticoagulation treatment given to hospitalized patients with a severe infection, unclear etiological factors of stroke, and disruption to global clinical trials. Further, few studies stratified stroke outcome data by ethnicity or age group, which has also been discussed in a separate published living systematic review on long COVID.7
Despite the variation in study methodology, much of the literature concluded that cerebrovascular complications may occur in patients with long COVID after being hospitalized for severe COVID infection, albeit at very low rates. With the limited evidence, there are no comparative data available versus the general population. In 3 of 4 studies that commented on the efficacy of administering prophylactic medication to prevent cerebrovascular complications posthospital discharge, authors suggested that extended prophylaxis may not incur a net clinical benefit. We call for good-quality randomized data to: (i) measure the incidence of stroke-related outcomes in long COVID in a controlled manner, and to (ii) inform recommendations for universal post-discharge prophylaxis.
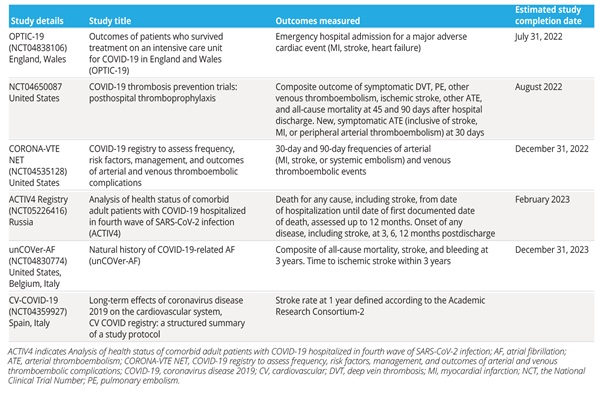
Further, we eagerly await data from planned European and US long COVID studies that intend to measure cerebrovascular-related outcomes as a primary or secondary endpoint by a future completion date (Table 1).
Table 1. Ongoing studies measuring stroke-related clinical outcomes in patients with long COVID
Management of long COVID and stroke-related neurological complications are not clearly defined in the available treatment guidelines
Given the insufficiency of published evidence measuring stroke-related outcomes in long COVID, we further reviewed treatment guidelines in this indication to check if any observed heterogeneity between clinical guidelines would corroborate some of the issues that we had previously observed in the coronavirus literature.
Figure 1 summarizes the available clinical guidelines and recommendations for patients with postacute COVID-19 for each stage of care, according to a mapped patient journey. Similar to our systematic literature review findings, the following points were concluded:
• Clinical guidelines inconsistently defined long COVID, with some guidelines suggesting that the definition will continue to evolve
• Some guidelines recommend prophylactic anticoagulation treatments to be prescribed for hospitalized patients with acute COVID-19 who are without any contraindication or need for higher dosage8,9
• Prophylactic anticoagulation treatments at hospital discharge were generally not recommended in the guidelines
• Many guidelines offered advice for all-cause complications in postacute COVID/long COVID, but there were limited specific recommendations for neurological complications including stroke
Figure 1. Summary of guidelines and recommendations for patients with postacute COVID-19
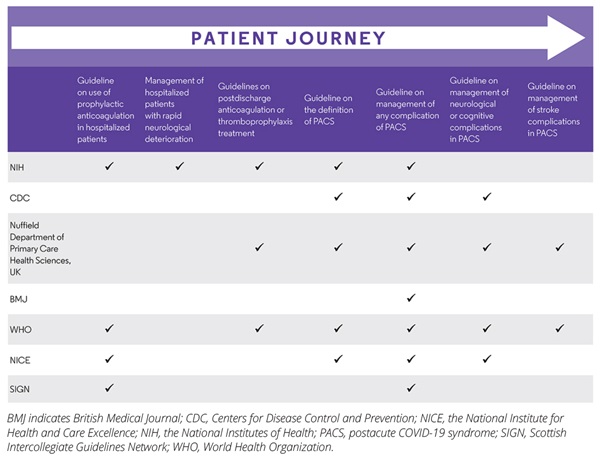
Taken together, the guidelines consider supportive management, symptom monitoring, and educating the patient on when to seek emergency care following hospital discharge. The National Institute for Health and Care Excellence recommends monitoring for “symptom alerts” of long COVID that occur within 1 to 2 weeks,10 and the Scottish Intercollegiate Guidelines Network recommends this at 6 weeks postdischarge.11
Conclusion
As interest in long COVID continues to evolve, future research may help us determine the true burden of stroke in long COVID. Although there are several published studies on postacute COVID-19, many large regional and global longitudinal follow-up studies have not included stroke outcomes in their scope. Even when they did, the stroke-related outcomes were not clearly stratified by the timepoints of occurrence (ie, whether these were since a severe infection or hospitalization).
A deeper understanding of the post-acute COVID-19 pathogenesis and a wider, more homogenous evidence base are required to assess whether there is any clinically significant relationship between long COVID and stroke. The systematic literature review process represents unbiased, high-quality evidence using robust methodologies that often drive clinical practice. The current systematic literature review highlights the possibility of cerebrovascular consequences of long COVID after a severe COVID-19 infection and is in contrast to other published systematic literature reviews that focus on cerebrovascular complications during a severe COVID-19 infection. Such evidence will presumably lead to clinical research with stroke-related endpoints, which will be essential to manage future pandemics of such magnitude.
At present, we feel that this assessment is hindered by limitations of the literature. Our findings call for prospective, robust, controlled trials that evaluate the cerebrovascular consequences of long COVID after a severe acute COVID-19 infection. Because the effects of the pandemic will be felt for years to come, there is an urgent need to synthesize emerging evidence regularly and systematically from ongoing and future global trials to document how the management of long COVID may evolve over time.
References
1. Nannoni S, de Groot R, Bell S, Markus H. Stroke in COVID-19: A systematic review and meta-analysis. Int J Stroke. 2020;16(2):137-149.
2. Ghannam M, Alshaer Q, Al-Chalabi M, Zakarna L, Robertson J, Manousakis G. Neurological involvement of coronavirus disease 2019: a systematic review. J Neurol. 2020 Nov;267(11):3135-3153.
3. Mullins CD, Drummond MF. The role of health economics and outcomes research in addressing coronavirus disease 2019 (COVID-19). Value Health. 2020. 1;23(11):1403-1404.
4. International Classification of Diseases for Mortality and Morbidity Statistics. 11th revision (ICD-11). World Health Organization. Published 2022. Accessed March 10, 2022. https://icd.who.int/browse11/l-m/en#/http://id.who.int/icd/entity/1442995018
5. Fleming C, Chakraborty A, Jaiswal T, Patel P, Nair S. Onset of stroke in patients with post-COVID-19 syndrome following hospitalisation for severe COVID-19 infection: a systematic literature review. Value Health. 2022;25(1):S121. https://www.ispor.org/heor-resources/presentations-database/presentation/euro2021-3407/114112
6. Nalbandian A, Sehgal K, Gupta A, et al. Post-acute COVID-19 syndrome. Nat Med. 2021;27(4):601-615. doi:10.1038/s41591-021-01283-z
7. Michelen M, Manoharan L, Elkheir N, et al. Characterising long COVID: a living systematic review. BMJ Glob Health. 2021;6(9):e005427. doi:10.1136/bmjgh-2021-005427
8. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. Published 2022. Accessed February 25, 2022. https://www.covid19treatmentguidelines.nih.gov/
9. Living guidance for clinical management of COVID-19. World Health Organization website. Published 2021. Accessed February 25, 2022. https://www.who.int/publications/i/item/WHO-2019-nCoV-clinical-2021-2
10. COVID-19 rapid guideline: managing the long-term effects of COVID-19. NICE guideline [NG188]. Published 2021. Accessed January 28, 2022. https://www.nice.org.uk/guidance/ng188
11. Managing the long-term effects of COVID-19. SIGN guideline. Published 2021. Accessed January 28, 2022. https://www.sign.ac.uk/our-guidelines/managing-the-long-term-effects-of-covid-19/

