Poster Session Recap: Cardiovascular Disorders
Tyler D. Wagner, PharmD, Virginia Commonwealth University School of Pharmacy, Richmond, VA, USA
This poster session showcased studies using a variety of methods, but all focused on cardiovascular disorders.
Completeness and Concordance Between Electronic Medical Records and Submitted Insurance Claims in German Hospitals Utilizing Percutaneous Left Ventricular Assist Devices: Considerations for Outcomes Research
Presenter: Jenny Unterkofler, Abiomed Europe GmbH, Aachen, Germany
Summary: A feasibility study designed to understand the concordance and potential loss of information in submitted insurance claims in comparison with the clinical data of patients treated with percutaneous left ventricular assist devices (pLVADs). Six clinical cases were extracted from electronic medical record systems and compared with submitted claims. Authors found that diagnostic and procedural concordance ranged from 70.59%-75.00%, and that missing information from claims was mainly related to timing of diagnoses and out-of-hospital medication regimens. Ultimately, while the fidelity of German claims data was moderately high and is acceptable in the complex therapeutic area of pLVADs, care should be taken to both collect additional data and match patients correctly to generate more reliable and granular datasets
Cost-Effectiveness of Initiating Antihypertensive Therapy With Single-Pill Combinations Versus Monotherapy in US Adults
Presenter: Alexis Bryan, Columbia University Medical Center, New York, NY, USA
Summary: Discrete event simulation was used to simulate blood pressure-related healthcare processes for 10,000 patients from the US National Health and Nutrition Examination Survey (NHANES) by projecting blood pressure changes, medication-related adverse events, cardiovascular disease events, and survival over a 10-year period. The authors compared the cost-effectiveness of initiating treatment with a single-pill combination containing 2 half-standard doses to 1 half-standard dose monotherapy. Overall, initiating a single-pill combination was estimated to cost $490 less and yield 0.02 more quality-adjusted life-years (QALYs) relative to monotherapy. Compared with monotherapy regimens, initiating treatment with single-pill combinations is expected to improve blood pressure outcomes, reduce cardiovascular disease events, reduce costs, and improve QALYs.
Cost-Effectiveness of Lisinopril and Carvedilol for Prevention of Trastuzumab-Induced Cardiotoxicity in US Adults With Early-Stage Breast Cancer
Presenter: Yehua Wang, University of Florida, College of Pharmacy, Gainesville, FL, USA
Summary: A randomized controlled trial has demonstrated that lisinopril and carvedilol reduced trastuzumab-induced cardiotoxicity (CTX) in a population of patients with early-stage breast cancer with previous anthracycline use. A Markov model was developed to simulate trajectories for patients between th3ree health states (ie, CTX-free, asymptomatic CTX, and symptomatic CTX) from a US payer perspective to assess the cost-effectiveness of lisinopril or carvedilol, as prophylaxis, versus no prophylaxis, among US patients with early-stage breast cancer receiving trastuzumab. The authors determined that based on a willingness-to-pay threshold of $50,000/QALY, lisinopril is a cost-effective prophylaxis (99% of iterations) against trastuzumab-induced CTX for patients with early-stage breast cancer in the United States. The higher drug price was a major impact factor for carvedilol’s economic efficiency, only being found to be cost-effective in 43% of the iterations, compared to no-prophylaxis.
Persistence to Treatment With Initially Prescribed Antiplatelet Agents for the Onset of Acute Coronary Syndrome
Presenter: Kibum Kim, PhD, University of Illinois at Chicago, Chicago, IL, USA
Summary: This is a retrospective analysis of EMR data from ~13,000 patients hospitalized with acute coronary syndrome (ACS) who had a prescription record for 1 of 3 oral anticoagulant agents (OAA) (ie, clopidogrel, prasugrel, and ticagrelor) within 7 days of hospital discharge. The objective was to determine the contemporary patterns of both OAA prescriptions and treatment switches made within the first 180 days of discharge. Clopidogrel dominated the initial OAA prescription following discharge (81%), with a total of 43% of patients switching to an alternative before the end of the 180-day follow-up period. Research demonstrated that despite the superior efficacy of the third-generation OAAs (prasugrel and ticagrelor) from clinical trial data, clopidogrel remained the preferred choice over the last decade.
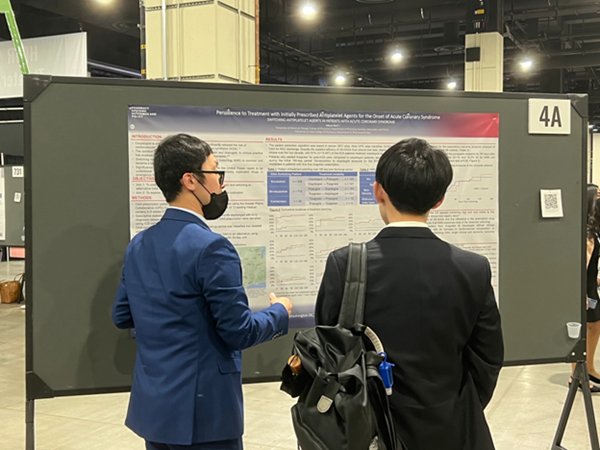
Kibum Kim discusses his research on contemporary patterns of oral anticoagulant agents in patients hospitalized with acute coronary syndrome.
The Effect of Preoperative Chest Physiotherapy on Oxygenation and Lung Functions Among Cardiac Surgery Patients: A Randomized Controlled Study
Presenter: Imre Boncz, PhD, University of Pécs, Pécs, Hungary
Summary: A randomized controlled trial of 100 adult patients with planned open heart surgery were blindly and randomly allocated into 2 groups; one group of patients who received a home chest physiotherapy program for 1 week preoperative plus traditional postoperative program, and the other group of patients who received only the traditional postoperative program. The majority of study patients received coronary artery bypass graft (64%) and significant differences were noted between study groups with regard to postoperative respiratory functions measurements (ie, FVC and FEV1) and O2 saturation at seven days (p-value <0.05).
The Effect of Team-Based Care Strategies on Systolic Blood Pressure at 6 Months: A Meta-Analysis
Presenter: Aditi Rao, MPH, Columbia University Medical Center, New York, NY, USA
Summary: A meta-analysis of randomized control trials published in the United States from 2003 to present that included patients with baseline systolic blood pressure (SBP) ≥140 mmHg or ≥130 mmHg in patients with diabetes or chronic kidney disease, compared team-based care with usual care, and had SBP outcomes reported at 6 months were analyzed. This meta-analysis assessed the impact of team-based care with and without self-monitoring of blood pressure or physician versus nonphysician titration of antihypertensive medications on SBP at 6 months. Fourteen studies were included in the analysis with a total sample size of 3305 participants. Rao et al found team-based care with antihypertensive medication titration by nonphysician team members appeared to be a particularly effective strategy to lower SBP.
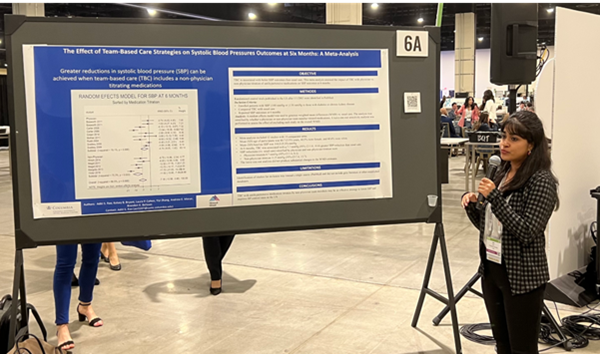
Aditi Rao presents her research on the effect of team-based care strategies on systolic blood pressure.

