Methodological Innovations to Deal With Disability in Cost-Effectiveness Analysis
Enrique M Saldarriaga, MS, The Comparative Health Outcomes, Policy, and Economics (CHOICE) Institute, University of Washington, Seattle, WA, USA; Mark Bounthavong, PharmD, PhD, UCSD Skaggs School of Pharmacy & Pharmaceutical Sciences, La Jolla, CA, USA
The Affordable Care Act (ACA) bans the use of quality-adjusted life-years (QALYs) in economic evaluations as it imposes a discounted value on disabled people and hence could be interpreted as discriminatory. At the core of the problem is the difficulty of QALYs to attain both horizontal and vertical equity. The former refers to the principle that people with similar needs should be treated similarly; vertical equity indicates that people with different needs should be treated differently. In particular, because QALYs discount the quality of life of people with disabilities health gains in this population are valued less and may be discriminatory.
Healthy Years in Total, use of ‘Shortfall’ in health technology assessment (HTA), and Generalized Risk-Adjusted Cost-Effectiveness (GRACE) are 3 methodological innovations that aim to resolve this problem. Charles Phelps, PhD (University of Rochester, USA) led an exciting discussion on the strengths and weaknesses of these new methods to overcome the shortcomings of the current QALY framework (Figure 1).
Figure 1. Session moderator and speakers.
 Clockwise: Darius Lakdawalla, Anirban Basu, Susan Griffin, and Chuck Phelps.
Clockwise: Darius Lakdawalla, Anirban Basu, Susan Griffin, and Chuck Phelps.
Anirban Basu, PhD (University of Washington, USA) presented “Dealing with Disability using Health Years in Total (HYT).” Basu argues that there is a corollary embedded in the horizontal equity principle: if similar gains in life expectancy or quality of life of 2 groups have to be valued equally, then different gains should be valued differently. HYT is designed to overcome both instances of horizontal equity by answering the counterfactual question: “for every treatment [available], what would have been the quality of life among patients getting the old intervention had those patients remained alive for more years?” and comparing that estimate to the factual (quantified) increase in quality of life associated with an intervention. Thus, HYT is the sum of life expectancy plus modified-QALYs, which are the number of expected QALY if a patient lived the maximum average life expectancy across any comparative treatment. One of the limitations of HYT is that it does not directly address vertical equity; however, it has the potential to do so provided there is enough information about the trade-offs between life expectancy and quality of life gains. On the other hand, one of the most important strengths of the HYT framework is that it can easily be incorporated with other methodologies, such as Shortfall and GRACE.
“The greater the shortfall, the greater the need or severity of the condition, and the willingness to pay is adjusted accordingly to reflect the higher value placed on populations with greater shortfalls." —Susan Griffin, PhD, MSc, BSc
Susan Griffin, PhD, MSc, BSc (University of York, UK) presented “Use of Shortfall in HTA Processes,” and provided an overview of European approaches to dealing with disability. Griffin noted that cost-effectiveness analysis does not occur in isolation but in combination with effectiveness evidence to inform reimbursement and treatment coverage of health technologies, and that the main issue with QALY is that it ignores the distribution of health that underlines the total quantity that we usually observe. Building on these concepts, the use of shortfalls in HTA seeks to weight the QALYs gained by different population groups according to a quantification of their needs or treatment gaps based on reduction in life expectancy due to illness or disability. Hence, “the greater the shortfall, the greater the need or severity of the condition,” and the willingness to pay is adjusted accordingly to reflect the higher value placed on populations with greater shortfalls. To incorporate the heterogeneity within the population, the life expectancy estimates should be different by age groups and gender. The shortfall can be estimated in “absolute terms” as the number of QALYs lost if the population did not have the condition or in “relative terms” as the percentage in the adjusted quality of life survival lost due to the condition. Both estimations can yield very different results as exemplified by the experience in the United Kingdom, where NICE updated its methods in January of 2022 to include both metrics in replacement of the “end of life modifier.” According to Griffin, this methodology "is not about the estimation but about the translation of health gains into social value." However, this implies that the metric carries some of the same issues associated with QALYs with respect to horizontal equity.
Darius Lakdawalla, PhD (USC Leonard D. Schaeffer Center for Health Policy and Economics, USA) presented “The GRACE Approach of HTA With Disability.” Lakdawalla started with a reflection on the fact that predictions in cost-effectiveness analyses appear to be at odds with patients’ (and societal) preferences with regard to the value placed on life expectancy and quality gains across populations, which generates political pushback as observed in the ACA. GRACE aims to resolve the issues associated with traditional quantification of QALYs, specifically regarding vertical equity, by recognizing that the value of health gains is diminishing in nature. Hence, people with lower quality of life will value any gain in health more than a healthier counterpart. The underlying assumption of the methodology is that disability leads to greater percentage loss of utility in the healthy (pre-disease) state than in the sicker (post-disease) state. The mathematical formulation of GRACE addresses this issue because sicker people receive higher weights by acknowledging that value in health gains are diminishing across health status. Thus, under the GRACE formulation “quality of life, improvements are always more valuable for people with disability than otherwise comparable people without it (Figure 2).
Figure 2. Under GRACE, quality of life gains are always more valuable to patients with disability.
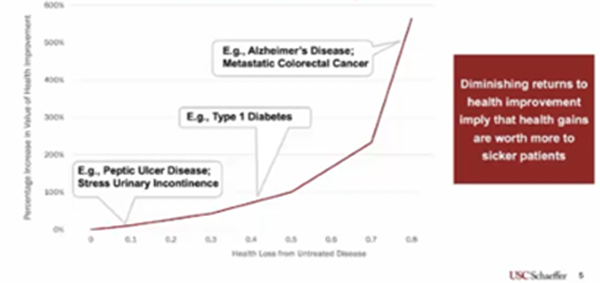
After the presentations, Phelps led a discussion that cemented the importance of these innovations to overcome the issues associated with traditional estimation of QALYs, including theory foundations of cost-effectiveness analysis, the differences between considering individual or societal preferences when defining health utility functions, and how to account for diminishing returns in health gains.

