Defining and Operationalizing No-Value Care
Trupti Dhumal, MS, BPharm, West Virginia University, Morgantown, WV, USA
The economic burden associated with low-value care is well established. Policy groups have identified the importance of reducing low-value services to lower costs and improve outcomes. In order to handle the challenges associated with healthcare costs, studies have identified low-value practices and recommendations, such as the Choosing Wisely program, to avoid unnecessary expenditure and make prudent decisions on the healthcare front. However, determination of “low-value” and operationalization of the definition varies highly depending on the level of subjectivity and individual biases based on what constitutes low-value.
The panel was moderated by Beth M. Beaudin-Seiler, PhD (Altarum, USA), who addressed the issue of inefficient spending and initiated an interactive discussion towards identifying a potential solution for policy makers. The general theme of the session was the need for a more concrete definition of “no-value care” and to identify what types of services would fall into this category.
“There is a great confusion among policy makers and decision makers between ‘cost-effectiveness’ and ‘cost saving.’ Cost effective services are not cost saving.” —A. Mark Fendrick, MD
The first speaker, A. Mark Fendrick, MD (University of Michigan, USA), began by emphasizing the need for a definition of no-value care. “There is a great confusion among policy makers and decision makers between ‘cost-effectiveness’ and ‘cost saving.’ Cost effective services are not cost saving,” said Fendrick.
Fendrick gave a comprehensive summary of value-based care and emphasized the need to shift the focus to no-value care (Figure 1). “Low value isn’t always no value or even low value—there is a clinical nuance. The clinical value of service depends on who gets it, how they get it, and who gave it…which needs to be analyzed by experts,” said Fendrick.
Figure 1. Getting past “low value” to “no value.”
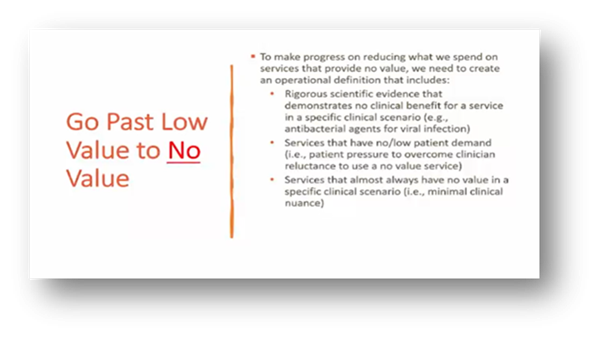
The use of an operational definition is needed to get past “low value” to “no-value.” The elements of the definition of no-value care include: (a) rigorous scientific evidence that demonstrated no clinical benefit, (b) services that have no/low value patient demand, and (c) services that almost always have no value in a specific clinical scenario. The PhRMA Foundation funded a project on operationalizing no-value care using a cost-effectiveness evidence registry from the Tufts Medical Center.
Peter J. Neumann, ScD (Tufts Medical Center, USA) introduced the elements of the registry and its use in understanding services and procedures to support the operationalization of a no-value care definition. The comprehensive database registry is housed at the Center for the Evaluation of Value and Risk in Health (CEVR) at Tufts Medical Center and contains information on more than 10,000 cost-utility analyses published between 1976 and 2020. Neumann stated that the registry’s objectives revolved around identifying society’s best opportunities for targeting resources to improve health, assisting policy makers in resource allocation decisions, and facilitating the use of standard methodologies (Figure 2).
Figure 2. Objectives of the CEVR registry.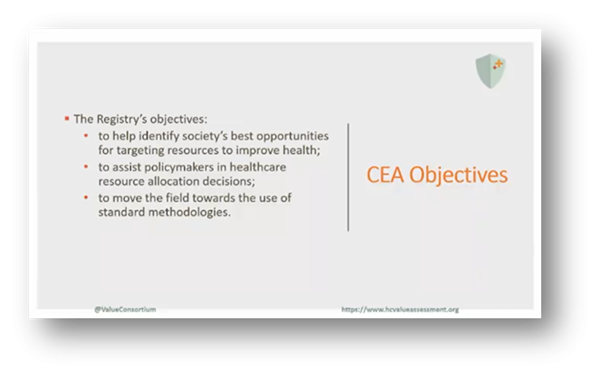
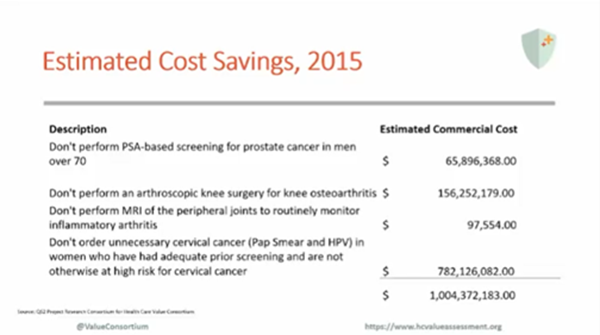
Beaudin-Seiler recommended evaluating the services in the Choosing Wisely program to see if they are necessary. Additionally, she explained the procedures of the project of utilizing cost-effectiveness analysis for no-value services. Out of 372 services, 38 services aligned with all 3 definition criteria and were segmented into 4 categories. Quantification of the 4 categories revealed an estimated expenditure of over $1 billion spent on no-value care services (Figure 3). Beaudin-Seiler reiterated the importance of the operationalization of the definition to cost-effectively spend money on useful services.
Figure 3. Estimated cost savings of eliminating no-value care.