An Invisible Burden: The Underrecognized Costs of Posttraumatic Stress Disorder Among Family/Friend Caregivers
Katherine Storey, Evidera, a PPD business, Montréal, QC, Canada; Karen Sandman, PhD, Evidera, a PPD business, Waltham, MA, USA
Introduction
According to the American Association for Retired Persons and the National Alliance for Caregiving, more than 1 in 5 Americans provided informal, unpaid caregiving services in 2020, caring in a nonprofessional capacity for an adult or child experiencing illness or disability.1 Often referred to as family/friend caregivers, the burden experienced by such individuals is well established, particularly as informal caregiving becomes more common due to an aging population, and in light of the COVID-19 pandemic, which not only increased the need for informal caregiving but also added to the weight carried by existing caregivers as many healthcare services became home-based.2-4 Across the age spectrum and around the world, unpaid caregivers provide necessary services to a family member, friend, or other individual with whom they are connected, helping them to potentially delay or avoid the need for admission to a long-term care facility.1 This scenario, while benefitting some caregivers by providing them with a sense of purpose and meaning, often results in disruptions to caregiver quality of life (QoL) and produces a considerable societal burden due to decreased productivity and disruptions to work.1,5-8 More specifically, family/friend caregivers experience impaired QoL, increased physical morbidity, lower health utility scores, higher rates of absenteeism and presenteeism, greater overall work impairment, and employment loss associated with the strain of caregiving.5-8 In addition, the caregiver population is reported to have impaired mental health and a high prevalence of psychiatric disorders, particularly clinical depression and anxiety disorders.7-9
"More than 1 in 5 Americans provided informal, unpaid caregiving services in 2020, caring in a nonprofessional capacity for an adult or child experiencing illness or disability."
One area of notable relevance to the caregiving population is trauma and stressor-related disorders, including posttraumatic stress disorder (PTSD). Based on the current diagnostic criteria for PTSD,10 caregivers are a population at risk. The event-related criterion for a PTSD diagnosis is Exposure to actual or threatened death, serious injury, or sexual violence. The first 2 experience qualifications for this criterion are (1) Directly experiencing the traumatic event(s) and (2) Witnessing, in person, the event(s) as it occurred to others.10,11 Traumatic event(s) relevant to the family/friend caregiver population may include their care recipient being diagnosed with a life-threatening illness, undergoing a life-threatening medical procedure, or being admitted to a hospital or intensive care unit (ICU), among other events.12-14 Moreover, caregivers may often witness serious injury or threatened death of their care recipient in situations such as dementia or mental illness and may themselves be the target of psychological abuse or serious physical threats in some cases.15,16
While several studies have explored the prevalence of PTSD in caregivers, it is likely to be underreported due to a number of interrelated factors, including difficultly distinguishing it from other disorders and/or more general emotional distress, a trend of PTSD under- and misdiagnosis in general, and diagnostic challenges relating to the nature of caregiving, where the focus of the caregiver and the healthcare team is primarily on the care recipient.17-20
PTSD has one of the highest economic burdens among mental disorders, as illustrated by a recent economic evaluation showing a per person excess cost of PTSD higher than what has been reported previously for anxiety, attention-deficit hyperactivity disorder (ADHD), or major depressive disorder.21 Comprising direct healthcare costs, direct nonhealthcare costs (eg, substance use disorder, disability), and indirect/societal costs (eg, unemployment, reduced productivity at work), the total costs related to PTSD were $232 billion in the 2018 US population, higher than those reported in other studies for anxiety, ADHD, bipolar disorder, or schizophrenia.21 To our knowledge, there have been no studies exploring the economic burden of PTSD specifically in the family/friend caregiver population. The ongoing research described below aims to better characterize this burden in order to facilitate further study on the economic and societal consequences of caregiver PTSD.22 Understanding this burden could help to inform education and awareness initiatives for healthcare providers and caregivers, and support the continued implementation of screening programs for early intervention, all of which have been recognized and recommended for at-risk caregiver populations but remain underutilized.4,18,20,23 Psychological therapies are the standard-of-care in PTSD, although pharmacotherapy may be used in some cases.11
"Family/friend caregivers experience impaired quality of life, increased physical morbidity, lower health utility scores, higher rates of absenteeism and presenteeism, greater overall work impairment, and employment loss associated with the strain of caregiving."
Prevalence of PTSD in Family/Friend Caregivers
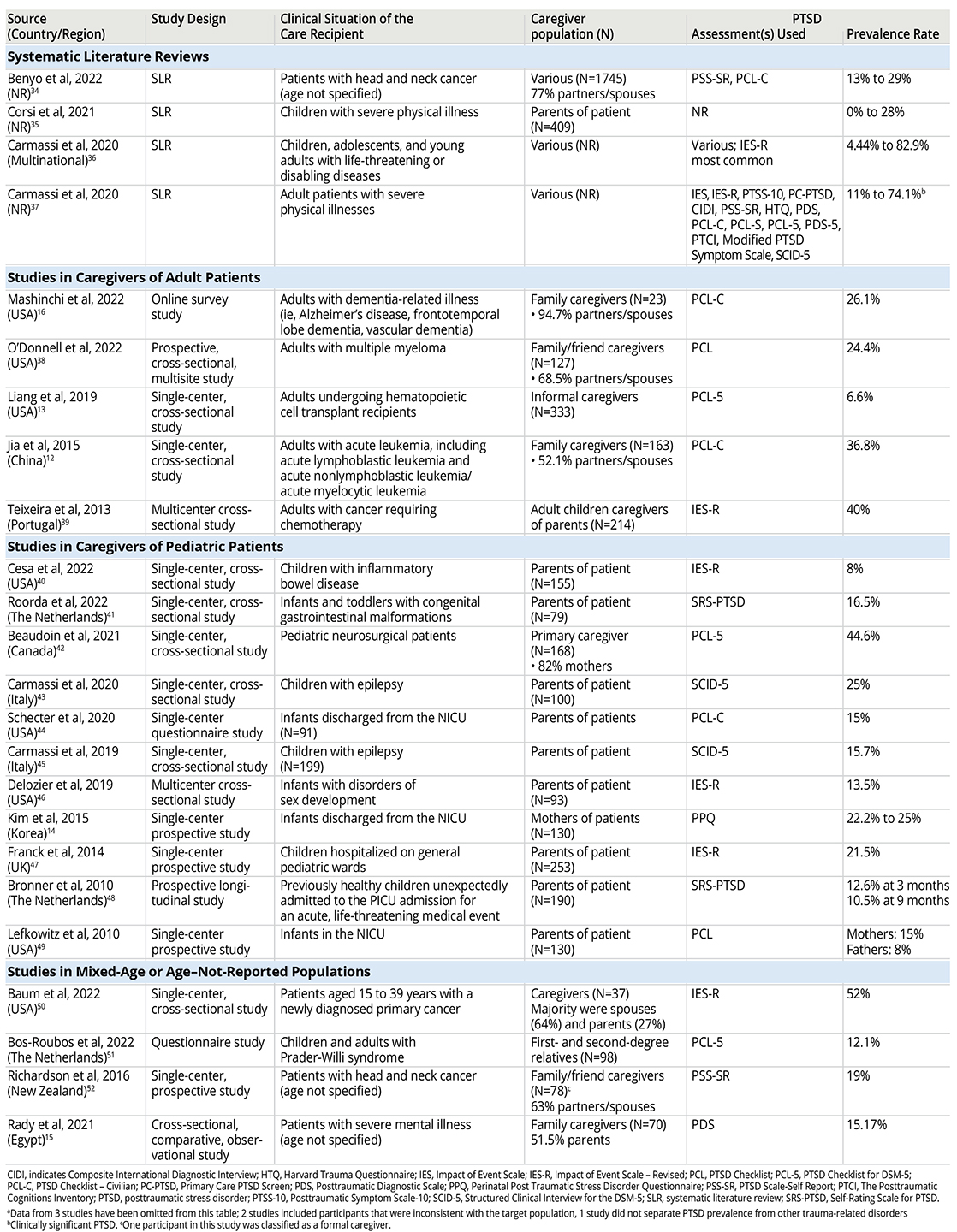
Our first step in assessing the economic burden associated with PTSD in caregivers was to estimate the prevalence rate. Using PubMed searches and a citation-mining approach, we conducted a targeted literature review of existing research on the prevalence of PTSD in family/friend caregivers globally as well as the costs associated with PTSD in civilian (nonmilitary) populations in the United States. Prioritizing the most recent studies (published since 2010), we identified 32 publications relevant to these topics—30 on the prevalence of PTSD in the target group of family/friend caregivers, and 2 reporting on the economic burden of PTSD in civilian populations. Our search for PTSD prevalence estimates was not limited to US studies in order to gather a large, diverse dataset. While the prevalence of PTSD is largely consistent across US and ex-US studies, further analysis would be needed to confirm that global PTSD prevalence estimates in family/friend caregiver populations are applicable to a US economic analysis.
In our review of the prevalence studies (Table), PTSD rates among family/friend caregivers were remarkably similar to those reported for military combat veterans. The 30 studies we identified included caregivers of patients within a variety of clinical situations, including severe mental illness, severe and/or chronic medical issues in both children and adults (including ICU and neonatal ICU admissions), dementia, and cancer. PTSD prevalence rates ranged from 3% to 82.9%, varying with patient age, patient diagnosis/clinical situation, and criteria used to define PTSD, among other factors. More than half of the 30 studies reported prevalence rates between 12% and 30% (Table), which closely mirrors the 11% to 30% range reported by the US Department of Veterans Affairs for PTSD among combat veterans.24 Of note, one study found no significant difference in the prevalence of PTSD between a population of familial caregivers and other at-risk groups such as emergency first responders, military veterans, and nurses.16 Although the identified studies utilized a variety of measures for the assessment of PTSD and its severity, the majority require moderate to severe symptoms in order to establish the presence of PTSD (Table).
Table. Studies reporting PTSD prevalence in family/friend caregiversa
Economic Burden of PTSD in Non-Military Populations To derive costs most closely in line with our target population, we limited the economic burden aspect of our search to nonmilitary populations in the United States. While literature describing costs in this population is limited, the most recent publication we identified reported an annual excess direct healthcare cost per patient of $13,016 for pooled Medicare, Medicaid, commercially insured, and uninsured groups in 2018 (adjusted to $13,933.47 in 2020 USD), using PTSD prevalence estimates in the US population.21 While the main drivers of direct healthcare costs in this study were not reported, direct healthcare costs included both medical and pharmacy components.21 The other identified study reported mean per patient annual direct costs of $18,753 and $10,960 for Medicaid (n=9114) and privately insured (n=9720) populations, respectively (2008 USD; adjusted to $26,726.51 and $15,620.04 in 2020 USD, respectively).25 The main cost drivers in Medicaid and privately insured patients were outpatient or other services (45.8% and 49.8%, respectively) and inpatient services (22.9% and 24.3%, respectively).25 In the absence of economic data specific to the family/friend caregiver population, we recognize that a key part of this research must be the contextualization of the caregiver population in the greater body of literature on economic outcomes in civilian PTSD.
Estimating the Economic Burden of PTSD in the Target Population
Using a simplistic model without severity/symptom matching, we calculated an annual excess direct healthcare cost of PTSD in the caregiving population of more than $74 billion USD for 2020 (Figure). In comparison, the estimated annual excess direct healthcare cost attributed to PTSD in 2018 in the US military population was ~$10 billion, or ~$10.7 billion in 2020 USD.21 While the present analysis focused solely on direct healthcare costs, the overall excess costs related to PTSD in the caregiving population are likely to be even greater if indirect costs such as lost productivity and unemployment are included. Incorporating indirect costs would require further analysis of the age distribution and demographic variables of family/friend caregivers.
Figure. Calculation of annual excess direct healthcare costs attributable to PTSD in the US population of family/friend caregivers
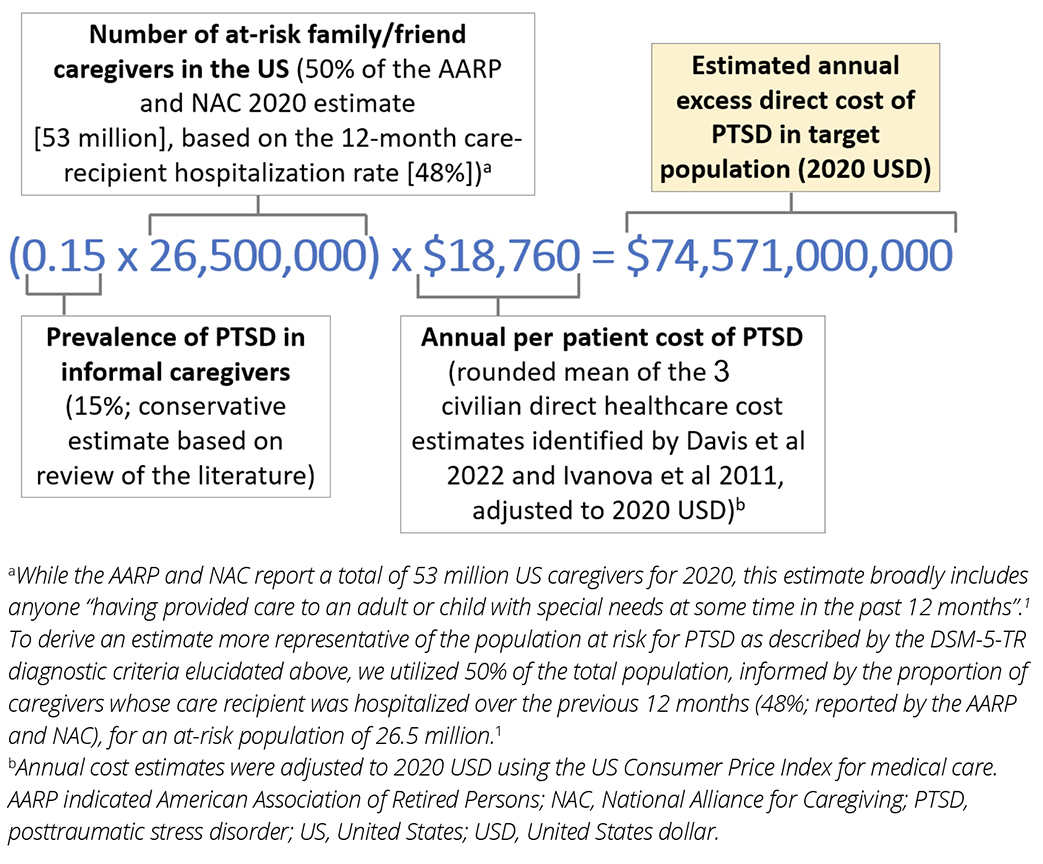
The initial model presented here is based on several assumptions that remain to be refined. The populations and methodologies in the studies used to estimate PTSD prevalence were diverse; the studies came from multiple countries/regions, and many were small, single-center studies. Thus, the model presented here assumes that the PTSD prevalence estimates identified in our literature review are applicable to the overall population of family/friend caregivers in the United States. Further, our analysis assumes that PTSD in family/friend caregivers incurs similar direct healthcare costs to other types of PTSD in US civilian populations. While these assumptions warrant further refinement, the magnitude of the preliminary cost figure—compounded by the steady growth of the caregiving population—underscores the need for further study to drive practice and policy.
Earlier in this report, we recognized the need to contextualize the caregiver population in the greater landscape of literature on PTSD, particularly in studies that report economic data. While the type of traumatic event and the severity of PTSD symptoms have both been found to influence economic outcomes, none of the studies we reviewed suggest that caregivers experience a mild form of PTSD relative to other sufferers.21,26 In fact, the diagnostic criteria utilized in most of the prevalence studies require PTSD symptoms of moderate to high severity. Serious outcomes associated with PTSD such as suicidal ideation and substance abuse have similarly been reported in the family/friend caregiver population.27-31
Moreover, while trauma-related outcomes are influenced by factors such as social and economic resources, age, gender, education level, personality and worldview, etc, posttraumatic trajectories of family/friend caregivers have been found to be consistent with those of the general population of individuals who experience a traumatic event.14,32,33 While these initial findings provide some insight, further study is needed to fully understand the place of the family/friend caregiver in the PTSD landscape, and to investigate whether there are any substantial differences relative to other populations for whom PTSD costs and outcomes have been reported.
"Annual excess direct healthcare cost of PTSD in the caregiving population of more than $74 billion USD for 2020."
Conclusion
Given that receiving a mental health diagnosis is associated with a dramatically increased likelihood of receiving appropriate treatment, the implications of PTSD underdiagnosis are grave; a lack of appropriate treatment has been linked to adverse outcomes including an increase in suicide attempts, greater impairments to QoL, and high healthcare costs, among others.19 Further, as the excess cost drivers in the 2 economic studies were primarily related to the use of medical services (including inpatient and outpatient services, other medical, and pharmacy costs), early intervention and treatment of PTSD have the potential to reduce the overall cost burden associated with this diagnosis. The substantial role that family/friend caregivers play in healthcare systems across the globe demonstrates the critical importance of their health and well-being, and recent recommendations suggest the implementation of educational and screening programs targeted at recognizing and treating mental health disorders in this population.1,4,20 By characterizing the economic burden of one common yet underrecognized diagnosis in these individuals, we hope to add to the existing body of research and help move the dial towards a more thorough integration of these recommendations into clinical practice and policy.
Acknowledgements: We would like to thank Timothy Peters-Strickland, MD, for sharing clinical insights; Donald Smith, PhD, and Marie Andrawes, PhD, for reviewing and providing input on the article; Héctor H. Toro-Diaz, PhD, for technical advice.
References
1. The National Alliance for Caregiving (NAC) and AARP. Caregiving in the US. 2020.
2. Dellafiore F, Arrigoni C, Nania T, et al. The impact of COVID-19 pandemic on family caregivers’ mental health: a rapid systematic review of the current evidence. Acta Biomed. 2022;93(S2):e2022154.
3. Lindt N, van Berkel J, Mulder BC. Determinants of overburdening among informal carers: a systematic review. BMC Geriatr. 2020;20(1):304.
4. Centers for Disease Control and Prevention. Caregiving for Family and Friends: A Public Health Issue. 2019.
5. Brannan AM, Brennan EM, Sellmaier C, Rosenzweig JM. Factors contributing to employment status over time for caregivers of young people with mental health disorders. Healthcare (Basel). 2022;10(8).
6. Igarashi A, Fukuda A, Teng L, Ma FF, Dorey J, Onishi Y. Family caregiving in dementia and its impact on quality of life and economic burden in Japan-web based survey. J Mark Access Health Policy. 2020;8(1):1720068.
7. Kehoe LA, Xu H, Duberstein P, et al. Quality of life of caregivers of older patients with advanced cancer. J Am Geriatr Soc. 2019;67(5):969-977.
8. Cohn LN, Pechlivanoglou P, Lee Y, et al. Health outcomes of parents of children with chronic illness: a systematic review and meta-analysis. J Pediatr. 2020;218:166-177.e162.
9. Malouf R, Harrison S, Burton HAL, et al. Prevalence of anxiety and post-traumatic stress (PTS) among the parents of babies admitted to neonatal units: a systematic review and meta-analysis. EClinicalMedicine. 2022;43:101233.
10. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed, text revision (DSM-5-TR). Washington, DC: American Psychiatric Publishing; 2022.
11. Hoskins M, Lewis C. Post-traumatic stress disorder. BMJ Best Practice. Published 2023. Accessed May 30, 2023. https://bestpractice.bmj.com/topics/en-us/430
12. Jia M, Li J, Chen C, Cao F. Post-traumatic stress disorder symptoms in family caregivers of adult patients with acute leukemia from a dyadic perspective. Psychooncology. 2015;24(12):1754-1760.
13. Liang J, Lee SJ, Storer BE, et al. Rates and risk factors for post-traumatic stress disorder symptomatology among adult hematopoietic cell transplant recipients and their informal caregivers. Biol Blood Marrow Transplant. 2019;25(1):145-150.
14. Kim WJ, Lee E, Kim KR, Namkoong K, Park ES, Rha DW. Progress of PTSD symptoms following birth: a prospective study in mothers of high-risk infants. J Perinatol. 2015;35(8):575-579.
15. Rady A, Mouloukheya T, Gamal E. Posttraumatic stress symptoms, quality of life, and stress burden in caregivers of patients with severe mental illness: an underestimated health concern. Front Psychiatry. 2021;12:623499.
16. Mashinchi GM, Hicks EC, Heppner H. The prevalence of PTSD among an online sample of US familial dementia caregivers. Adv J Social Sci. 2022;11(1):43-51.
17. Grunberg VA, Geller PA, Hoffman C, Njoroge W, Ahmed A, Patterson CA. Parental mental health screening in the NICU: a psychosocial team initiative. J Perinatol. 2022;42(3):401-409.
18. Salley CG, Axelrad M, Fischer E, Steuer KB. But parents need help! Pathways to caregiver mental health care in pediatric hospital settings. Palliat Support Care. 2022:1-7.
19. Gagnon-Sanschagrin P, Schein J, Urganus A, et al. Identifying individuals with undiagnosed post-traumatic stress disorder in a large United States civilian population: a machine learning approach. BMC Psychiatry. 2022;22(1):630.
20. National Alliance for Caregiving. Caring For The Caregiver: Incentivizing Medical Providers to Include Caregivers as Part of the Treatment Team. 2021.
21. Davis LL, Schein J, Cloutier M, et al. The economic burden of posttraumatic stress disorder in the United States from a societal perspective. J Clin Psychiatry. 2022;83(3).
22. Storey K, Sandman K. Post-traumatic stress disorder (PTSD) in caregivers: review of the existing evidence and proposed framework to estimate economic burden. ISPOR 2023; May 7-10, 2023; Boston, MA.
23. Bloyd C, Murthy S, Song C, Franck LS, Mangurian C. National cross-sectional study of mental health screening practices for primary caregivers of NICU infants. Children (Basel). 2022;9(6).
24. National Center for PTSD. How Common is PTSD in Veterans? US Department of Veterans Affairs. Updated February 3, 2023. Accessed March 14, 2023. https://www.ptsd.va.gov/understand/common/common_veterans.asp.
25. Ivanova JI, Birnbaum HG, Chen L, et al. Cost of post-traumatic stress disorder vs major depressive disorder among patients covered by medicaid or private insurance. Am J Manag Care. 2011;17(8):e314-323.
26. von der Warth R, Dams J, Grochtdreis T, König HH. Economic evaluations and cost analyses in posttraumatic stress disorder: a systematic review. Eur J Psychotraumatol. 2020;11(1):1753940.
27. Solimando L, Fasulo M, Cavallero S, et al. Suicide risk in caregivers of people with dementia: a systematic review and meta-analysis. Aging Clin Exp Res. 2022;34(10):2255-2260.
28. LeBouthillier DM, McMillan KA, Thibodeau MA, Asmundson GJ. Types and number of traumas associated with suicidal ideation and suicide attempts in PTSD: findings from a US nationally representative sample. J Trauma Stress. 2015;28(3):183-190.
29. Denham AMJ, Wynne O, Baker AL, et al. An online cross-sectional survey of the health risk behaviours among informal caregivers. Health Promot J Austr. 2020;31(3):423-435.
30. Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Prevalence and Axis I comorbidity of full and partial posttraumatic stress disorder in the United States: results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. J Anxiety Disord. 2011;25(3):456-465.
31. Hernandez Chilatra J, Browning W, Wang D, Pickering C. Risk factors for hazardous drinking among dementia family caregivers [Abstract]. Innovation in Aging. 2022;6(S1):765.
32. Bonanno GA, Westphal M, Mancini AD. Resilience to loss and potential trauma. Annu Rev Clin Psychol. 2011;7:511-535.
33. Opsomer S, Lauwerier E, De Lepeleire J, Pype P. Resilience in advanced cancer caregiving. A systematic review and meta-synthesis. Palliat Med. 2022;36(1):44-58.
34. Benyo S, Phan C, Goyal N. Health and well-being needs among head and neck cancer caregivers: a systematic review. Ann Otol Rhinol Laryngol. 2023;132(4):449-459.
35. Corsi M, Orsini A, Pedrinelli V, et al. PTSD in parents of children with severe diseases: a systematic review to face Covid-19 impact. Ital J Pediatr. 2021;47(1):8.
36. Carmassi C, Dell’Oste V, Foghi C, et al. Posttraumatic stress reactions in caregivers of children and adolescents/young adults with severe diseases: a systematic review of risk and protective factors. Int J Environ Res Public Health. 2020;18(1).
37. Carmassi C, Foghi C, Dell’Oste V, Bertelloni CA, Fiorillo A, Dell’Osso L. Risk and protective factors for PTSD in caregivers of adult patients with severe medical illnesses: a systematic review. Int J Environ Res Public Health. 2020;17(16).
38. O’Donnell EK, Shapiro YN, Yee AJ, et al. Quality of life, psychological distress, and prognostic perceptions in patients with multiple myeloma. Cancer. 2022;128(10):1996-2004.
39. Teixeira RJ, Pereira MG. Growth and the cancer caregiving experience: psychometric properties of the Portuguese Posttraumatic Growth Inventory. Fam Syst Health. 2013;31(4):382-395.
40. Cesa KT, Cunningham CA, Noll RB, Kim SC. Parental distress in pediatric inflammatory bowel diseases: associations with time from diagnosis, disease activity, and demographic factors. Crohns Colitis 360. 2022;4(2):otac019.
41. Roorda D, van der Steeg AFW, van Dijk M, et al. Distress and post-traumatic stress in parents of patients with congenital gastrointestinal malformations: a cross-sectional cohort study. Orphanet J Rare Dis. 2022;17(1):353.
42. Beaudoin W, Moore H, Bliss L, Souster J, Mehta V. Prevalence of post-traumatic stress disorder in caregivers of pediatric neurosurgical patients. Childs Nerv Syst. 2021;37(3):959-967.
43. Carmassi C, Corsi M, Bertelloni CA, et al. Post-traumatic stress spectrum symptoms in parents of children affected by epilepsy: gender differences. Seizure. 2020;80:169-174.
44. Schecter R, Pham T, Hua A, et al. Prevalence and longevity of PTSD symptoms among parents of NICU infants analyzed across gestational age categories. Clin Pediatr (Phila). 2020;59(2):163-169.
45. Carmassi C, Corsi M, Bertelloni CA, et al. Post-traumatic stress and major depressive disorders in parent caregivers of children with a chronic disorder. Psychiatry Res. 2019;279:195-200.
46. Delozier AM, Gamwell KL, Sharkey C, et al. Uncertainty and posttraumatic stress: differences between mothers and fathers of infants with disorders of sex development. Arch Sex Behav. 2019;48(5):1617-1624.
47. Franck LS, Wray J, Gay C, Dearmun AK, Lee K, Cooper BA. Predictors of parent post-traumatic stress symptoms after child hospitalization on general pediatric wards: a prospective cohort study. Int J Nurs Stud. 2015;52(1):10-21.
48. Bronner MB, Peek N, Knoester H, Bos AP, Last BF, Grootenhuis MA. Course and predictors of posttraumatic stress disorder in parents after pediatric intensive care treatment of their child. J Pediatr Psychol. 2010;35(9):966-974.
49. Lefkowitz DS, Baxt C, Evans JR. Prevalence and correlates of posttraumatic stress and postpartum depression in parents of infants in the Neonatal Intensive Care Unit (NICU). J Clin Psychol Med Settings. 2010;17(3):230-237.
50. Baum LV, Koyama T, Schremp EA, et al. Posttraumatic stress symptoms and financial toxicity among adolescent and young adult oncology patients and their caregivers at cancer diagnosis. Cancer. 2022;128(10):2005-2014.
51. Bos-Roubos A, Wingbermühle E, Biert A, de Graaff L, Egger J. Family matters: trauma and quality of life in family members of individuals with Prader-Willi syndrome. Front Psychiatry. 2022;13:897138.
52. Richardson AE, Morton RP, Broadbent EA. Illness perceptions and coping predict post-traumatic stress in caregivers of patients with head and neck cancer. Support Care Cancer. 2016;24(10):4443-4450.

