Overcoming Vaccine Hesitancy: Injecting Trust in the Community
Following a concerted global effort, multiple COVID-19 vaccines have been approved and are currently being administered around the world. While we celebrate this achievement, it represents only the beginning of an equally arduous process. To end this pandemic, a sufficiently large proportion of the global population—billions and billions of people—must be vaccinated.
While nations struggle with manufacturing and supply-chain logistics, the growing worldwide distrust in immunization and the rise of vaccine hesitancy may prove even more challenging. Governments, public health officials, and advocacy groups must be prepared to address vaccine hesitancy to ensure adoption of novel vaccines, achieve broad population immunity, and help us return to more normal lives. Unless the origins of such wide variation in willingness to accept a COVID-19 vaccine is better understood and addressed, differences in vaccine coverage between countries could potentially delay global control of the pandemic and the ensuing societal and economic recovery.
For this article, William Schaffner, MD, Lynn Field-Harris, MPA, and Nelly Salgado de Snyder, PhD shared their thoughts on vaccine hesitancy, differences across populations, and possible ways real-world evidence may help to address vaccine hesitancy.
The Complicated Construct
Vaccine hesitancy—a patient-level reluctance or refusal to receive a vaccination—is a deeply complex and context-specific construct, influenced strongly by personal experiences and belief systems.1 It threatens to not only reverse progress made in tackling vaccine-preventable diseases (eg, measles), but also derail efforts to control the current COVID-19 pandemic.
Despite vaccinations having long been heralded as providing one of the most cost-effective ways of avoiding disease, preventing 2 to 3 million deaths a year, public doubt and unease continues to grow. In 2019, following a 30% increase in the number of measles cases globally, the World Health Organization highlighted the dangers of vaccine hesitancy as one of the top 10 health threats joining air pollution, climate change, and HIV/AIDS.
The enormously successful history of vaccines may be contributing to increasing levels of hesitancy. Previously devastating diseases, such as polio and smallpox, are long forgotten, leading some patients to minimize the potential threats of vaccine-preventable diseases as they weigh the potential risks and benefits of newer vaccines.2
Furthermore, some patients may overestimate risks associated with current vaccines due to misinformation obtained through misleading or erroneous social media and other poorly vetted sources. Despite rapid spread of the current COVID-19 contagion, misinformation is spreading at an even faster rate. Misinformation creates barriers to universal vaccination, obfuscating vaccination benefits and emphasizing the adverse effects of vaccination, thus impeding patient understanding and overall buy-in.3 Not only are these sources free from editorial oversight, but users may also self-select content streams, which may contribute to ideological isolation and further limit access to accurate information.
Who Is Prone to Hesitancy?
Recent global surveys of COVID-19 vaccine hesitancy reveal large differences by country. A June 2020 survey of 13,426 people from 19 countries found that while 71.5% of participants voiced a willingness to take a COVID-19 vaccine, rates by country varied from almost 90% in China to less than 55% in Russia.4
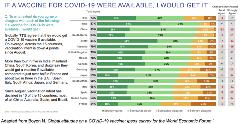
Figure. Global survey of 18,526 adults in 15 countries regarding willingness to take the COVID-19 vaccine.
Political climate may also influence vaccine hesitancy. Soon-to-be-published research identified a highly significant positive association between support for populist parties and skepticism of vaccine importance of effectiveness.6 Authors argue that vaccine hesitancy and political populism are both rooted in a profound distrust in elites and experts on both ends of the political continuum.
The Kaiser Family Foundation monitors attitudes in the United States towards COVID-19 vaccinations. Its December 2020 report found that 71% of respondents would probably or definitely receive the COVID-19 vaccine, while roughly a quarter of respondents remain hesitant. Within this December report, vaccine hesitancy varied by political leaning (higher for Republicans versus Democrats) and residency (higher rates for rural versus urban residents).
Racial Differences in Vaccine Perception
Perhaps the most important revelation in the Kaiser Family Foundation’s December report concerned differences in vaccine hesitancy by race. Roughly a third of Black adults (35%) stated that they definitely or probably would not get vaccinated. The COVID Collaborative, a nonprofit coalition made up of Langer Research Associates, Unidos US, and the National Association for the Advancement of Colored People, examined beliefs held by Blacks and Latinos regarding the safety and effectiveness of COVID-19 vaccines, finding 86% of Black and 66% of Latino respondents doubted vaccine safety, while 82% and 60% doubted effectiveness.
These racial differences are particularly troubling given that vaccine hesitancy affects those populations that are also disproportionately suffering the impacts of COVID-19. To prevent widening health disparities, it is critical to address vaccine hesitancy within these groups.
Deep-Seated Mistrust in the Process
“I really understand the whole issue of hesitancy,” shared Lynn Fields-Harris, MPA, former executive director of Center in the Park, a community center serving a predominantly Black population of older adults in Philadelphia, Pennsylvania. “I understand not so much fear of the vaccine and fear of COVID-19, but the distrust in government and the medical community, which has been exacerbated by the pandemic, laying bare the racism and inequity systematized in this country.”
The significant mistrust held by many communities of color of public health officials, policy makers, and health providers continues today. The long history of both abuse and exclusion of people of color continues to erode patient trust, as Fields-Harris emphasized the ongoing impact of the Tuskegee Syphilis Study. [Editor’s Note: “The Tuskegee Study of Untreated Syphilis in the Negro Male” was a study conducted between 1932 and 1972 by the United States Public Health Service and the Centers for Disease Control and Prevention.] “I feel like the struggle for communities of color is on so many levels the focus in terms of rebuilding trust,” she said. “It is really going to have to be something visible. Something tangible that people can see is moving in the right direction.”
"Despite vaccinations having long been heralded as providing one of the most cost-effective ways of avoiding disease, preventing 2 to 3 million deaths a year, public doubt and unease continues to grow."
William Schaffner, MD, professor of Preventive Medicine and Health Policy, Division of Infectious Diseases at Vanderbilt University, understands why some populations may be resistant to vaccines. “In the interest of equity and appropriate public health response, you reach out to minority populations to make sure that they’re vaccinated, and they may respond in a way that you hadn’t anticipated, saying ‘Wait a minute, do you want us to go first? Oh, once again, you’re experimenting on us.’” This, he noted, may lead many within this population to opt out of vaccinations, waiting instead for more safety evidence.
To help reassure Black Americans of the safety of COVID-19 vaccines, the National Medical Association, a professional society of African American doctors, conducted its own review of vaccine data, endorsing the emergency authorizations of both the Moderna and Pfizer/BioNTech vaccines.
Nelly Salgado de Snyder, PhD, spoke to COVID-19 vaccine attitudes held by Mexicans residing in Mexico versus those residing in the United States. Salgado de Snyder is a professor and senior researcher in medical sciences at the National Institute of Public Health of Mexico and currently is a Latino Research Institute Fellow at the University of Texas studying health access for Mexican immigrants in the United States. She noted that antivaccine views in Mexico are relatively rare given the country’s history of successful universal vaccination campaigns. “Overall, people in Mexico are receptive to vaccines,” she said. “Mexican immigrants in the United States experience far higher levels of hesitancy driven by both vaccine misinformation and by mistrust of the government. The problem with immigrants who live in the United States is that they have limited access to health information and they do not trust the government or institutions in general.”
Salgado de Snyder sees the US political climate regarding immigration and undocumented workers fueling immigrants’ mistrust of public health and other institutional organizations, leading to the belief that these institutions may be a threat to their well-being. She shared an example of vaccine misinformation received through social media messages. “Social media posts state, ‘The vaccine is a plot! They are injecting you with the virus because they want to get rid of you and all the immigrants! You are undesirable in this country!’”
A recent Kaiser Family Foundation survey supported this view, finding 74% of Hispanic respondents in the United States feel hesitant or resistant to the vaccine.7 Yet, Salgado de Snyder said that hesitancy among immigrants is often higher in men. She noted that immigrant men are particularly prone to vaccine hesitancy given their concerns about lost income from time spent seeking vaccinations.
Finally, trust in public health organizations has been further eroded by the politicization of the COVID-19 pandemic. In the United States, the former administration’s support for the use of hydroxychloroquine in treating COVID-19 despite there being no reliable supporting evidence of its efficacy or safety, coupled with the “warp speed” vaccine development timeline has heightened suspicions of how safe and effective the vaccines are.
Using Real-World Evidence to Open the Door to Trust
In the current battle against COVID-19, real-world evidence has helped accelerate the development of safe and effective vaccines, providing critical evidence needed for emergency use authorization. And through projects such as the Vaccine Safety Datalink, a partnership between the Centers for Disease Control and 8 health plans, and the Post-Licensure Rapid Immunization Safety Monitoring System, a part of the US Food and Drug Administration’s Sentinel Initiative, real-world evidence continues to be used track the safety of new vaccines.8,9
In addition to these ongoing surveillance measures, real-world evidence may also help address vaccine hesitancy by providing the necessary information about the safety and efficacy of new COVID-19 vaccines needed to help reassure patients. Possible ways that real-world evidence may contribute include:
• Conducting culturally responsive assessment of vaccine efficacy and safety within specific subpopulations, such as Black or Latino populations
• Examining safety and efficacy in patients with rare conditions (eg, sickle cell disease) or other comorbid conditions
• Addressing fertility/reproduction concerns
• Conducting comparisons of different vaccines within subpopulations. Are all COVID-19 vaccines equally safe and effective in all subpopulations?
The determinants of vaccine hesitancy differ depending on the cultural, societal, and personal beliefs; geographic region; and sociodemographic characteristics. They may evolve as misinformation spreads. Therefore, ongoing surveillance is needed so researchers can understand what information is needed to tailor evidence-based strategies to overcome the problem with sustainable interventions.
In designing research strategies to alleviate vaccine hesitancy, Schaffner emphasized the need to understand the core reasons behind individual fears. “You have to respect that it’s perfectly reasonable to be skeptical, hesitant, and concerned. You have to recognize that there are many people who may not read the paper every day or read the scientific literature.” He continued, “Once you recognize that skepticism is reasonable and is an appropriate human response, you then open up your mind and begin to ask, ‘What evidence may help settle their fears?’”
Fields-Harris agreed with this need for researchers to understand the core concerns of these communities. “I do think that mistrust is deeply ingrained. Researchers and scientists must gain an understanding of the communities so there can be some kind of engagement.”
“There’s a great feeling that we are responsible for one another, that together we’re willing to make that sacrifice for the safety of other people.” —Lynn Field-Harris, MPA
Importance of the Right Message and the Right Messenger
Hesitancy may persist even with more culturally sensitive messages—accurate and relevant information that is free from political influence. The knowledge-deficit approach to address vaccine hesitancy has shown limited effect in changing minds given the complex mix of cognitive, emotional, cultural, social, spiritual, and political factors that influence vaccination choices.10
“Information is necessary, but not sufficient to change people’s attitudes and behavior,” said Schaffner. “You have to change their attitudes. And that’s where you need to be comforting and reassuring. I keep using these words, ‘comfort and reassurance’ more than facts. When we lead with facts often it is not the best way to start.”
Schaffner, Fields-Harris, and Salgado de Snyder emphasized the importance of the right messenger together with the right message when addressing vaccine hesitancy such as a respected, trusted source in their community. Both Fields-Harris and Salgado de Snyder highlighted the influence religious leaders and teachers could have in alleviating vaccine hesitancy. Fields-Harris said, “Information around what the vaccine is, what the impact is, was much more readily accepted by peer-to-peer education and awareness.” Schaffner added that vaccine messaging may need to reach beyond standard public health outlets, using instead neighborhood barbershops or beauty shops. And Salgado de Snyder stressed the importance that all vaccine messaging be translated into native languages and be accessible to even a low-literacy public.
Hope for Future Community Support
Promisingly, the people we spoke to for this article were hopeful that by addressing vaccine hesitancy, wider community support for COVID-19 vaccines may drive vaccination campaigns. “My hope is that as everybody else gets vaccinated and we begin to see beneficial effects of the vaccine, some of those hesitant people will be brought in. They want to be part of the group,” said Schaffner.
“If people feel that taking the vaccine will have a broader impact beyond themselves, I believe they will be more inclined to do it,” added Fields-Harris. “There’s a great feeling that we are responsible for one another, that together we’re willing to make that sacrifice for the safety of other people.”
References
1. Amin AB, Bednarczyk RA, Ray CE, et al. Association of moral values with vaccine hesitancy. Nat Hum Behav. 2017;1:873-880.
2. Rosenberg C. What is an epidemic? AIDS in historical perspective. Daedalus. 1989;118(2):1-17.
3. Tustin JL, Crowcroft NS, Gesink D, et al. User-driven comments on a Facebook advertisement recruiting Canadian parents in a study on immunization: content analysis. JMIR Public Health Surveill. 2018:4(3):e10090.
4. Lazarus JV, Ratzan S, Palaye A, et al. A global survey of potential acceptance of a COVID-19 vaccine. Nat Med. Published October 2020. https://doi.org/10.1038/s41591-020-1124-1129. Accessed January 14, 2021.
5. Boyon N. Global attitudes on a COVID-19 vaccine: Ipsos survey for the World Economic Forum. Published November 5, 2020. https://www.ipsos.com/en/global-attitudes-covid-19-vaccine-october-2020. Accessed January 20, 2021
6. Kennedy J. Populist politics and vaccine hesitancy in Western Europe: an analysis of national-level data. Eur J Public Health. 2019:29(3);512-516.
7. Kearney A, Lopes L, Brodie M. Vaccine Hesitancy Among Hispanic Adults. The Kaiser Family Foundation. Published January 14, 2021. www.kff.org/coronavirus-covid-19/poll-finding/vaccine-hesitancy-among-hispanic-adults/. Accessed January 22, 2021.
8. Vaccine Safety Datalink. Centers for Disease Control and Prevention. Updated August 24, 2020. cdc.gov/vaccinesafety/ensuringsafety/monitoring/vsd/. Accessed January 22, 2021.
9. Vaccine Safety. US Department of Health and Human Services. Updated February 2020. vaccines.gov/basics/safety. Accessed January 22, 2021.
10. Dube E, Laberge C, Guay M, Bramadat P, Roy R, Bettinger J. Vaccine hesitancy: an overview. Hum Vaccine Immunother. 2013;9(8):1763-1773.
About the Author
Michele Cleary is a HEOR writer in Minneapolis, MN.
Explore Related HEOR by Topic

