Preventing the Breakdown of the Healthcare System: How to Use the SIR Model to Allocate Medical Resources Better
Aakash Bipin Gandhi, BPharm, Department of Pharmaceutical Health Services Research, University of Maryland, Baltimore, MD, USA; and Vasco Pontinha, MPharm, MA, Department of Pharmacotherapy and Health Outcomes, Virginia Commonwealth University School of Pharmacy, Richmond, VA, USA
The COVID-19 pandemic has created a unique need for a high quantity of healthcare resources. “In order to prevent the breakdown of the healthcare system, we need to promote the efficient allocation of healthcare resources”. With this statement, Wai-kit Ming, MD, PhD, MPH, MMSc, EMBA, Jina University, Guangzhou, China, kicked of an exciting session on how researchers can use infectious disease models like SIR models to help speculate medical resource needs during the COVID-19 pandemic.
“In order to prevent the breakdown of the healthcare system, we need to promote the efficient allocation of healthcare resources.”—Wai-kit Ming, MD, PhD, MPH, MMSc, EMBA
Panelist Jian Huang, PhD, MPH, Imperial College London, London, United Kingdom, shed some light on the working of the SIR model in helping speculate the need for healthcare resources during the COVID-19 epidemic in Wuhan. “The classical SIR model consists of individuals that can be divided into three compartments: Susceptible, infected, and removal (die/recover).” The SIR model helps researchers visualize how individuals move across these three compartments. Some key assumptions of the SIR model are that the number of individuals across the three compartments remain constant or that there is a constant rate of movement for individuals across the three compartments.
Some key model inputs of the SIR model include the total population size, number of daily cases confirmed, number of daily cases admitted to the intensive care unit, disease diagnosis rate, disease infection rate, disease recovery rate, and the risk of mortality among hospitalized patients. While the objective of the model is to determine the resource needs of the healthcare system, it has certain limitations. First, due to the lack of comprehensive knowledge on the virus and infection rates, there still exists a high magnitude of uncertainty around the model findings. Hence, as model inputs are updated, it is important to revisit the model to report real-time results that may have an impact on policy making.
In addition to predictive models that can help quantify the demand of healthcare resources, public health measures consisting of non-pharmaceutical interventions should be considered to avoid the breakdown of the healthcare systems. Zonglin He, MBBS, International school, Jinan University, Guangzhou, China, discussed the several interventions that some countries have implemented to curtail the breakdown of the healthcare system. Briefly, these interventions encompass imposing social distancing guidelines, travel bans, implementation of massive screening protocols, and mandatory use of facemasks (indoor and outdoor). Nevertheless, the draconian nature of these measures also has societal consequences.
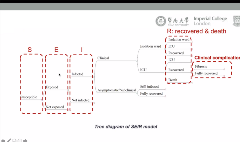
Using the SIR model, Zonglin discussed how the cost-effectiveness of these public health measures can be calculated. Using a Markov model, in which people can transition from at risk states, to diseased, recovered, or dead stages, three public health interventions were compared (Figure 1). These scenarios pertain to the actual public health measures that were implemented in Wuhan, China: a) no restrictions; b) full lockdown (including public transportation shutdown, closure of public places, and compulsory face mask-wearing); and c) short-term lockdown, that included public transportation suspension and closure of public places until a massive screening program is put in place. According to Zonglin, the results that compared to no restrictions, short-term lockdown are the dominant intervention, yielding the largest savings in direct medical costs, the most cases and deaths averted, and the most quality of life years (QALY) saved.
Figure 1. Model considered to evaluate the cost-effectiveness of three different public health measures.
In the absence of treatments or vaccines during this global pandemic, modeling nonphharmaceutical public health measures is particularly relevant to inform policy decision-making. Casper J.P. Zhang, PhD, MPH, School of Public Health, LKS Faculty of Medicine, The University of Hong Kong, Hong Kong, China, discussed and compared the results of lockdowns imposed in three countries: the United Kingdom, Australia, and China. The publicly available data shows that the United Kingdom imposed the less stringent lockdowns of the three countries: currently, the United Kingdom is facing a massive second wave of cases. Thus, the British government imposed a second lockdown planned to end in early December.
“The Hubei province does not have one single active case or community transmission of the virus.”—Casper J.P. Zhang, PhD, MPH
The state of Victoria in Australia saw a massive second wave in early July, which resulted in the decision to impose a strict lockdown that lasted for 111 days. The latest data available shows that this region has not seen one single case of COVID-19. China was the country that imposed the most draconian measures to curtail the transmission of the virus. In fact, the Chinese government decided to “eliminate the curve instead of simply flatten it.” Despite its large population, Zhang showed how the Hubei only saw a single wave of infections and, currently, the Hubei province does not have one single active case or community transmission of the virus.
He concluded that SIR modeling is a helpful tool for prediction of disease transmission and that it is also beneficial for planning public health measures and effectively allocate healthcare resources.

