Integrating Patient Preference Into HTA
Felix Wolfrum, MSc, and Christian Lamping, MSc, Department of Applied Natural Sciences, TH Köln - University of Applied Sciences, Cologne, Germany
The moderator Esther de Bekker-Grob, PhD, Erasmus University Rotterdam, Rotterdam, The Netherlands introduced the participants with a brief introduction on the background of patient preferences and led them consistently through the interactive session (Figure 1). The purpose of the session was to discuss the opportunities and challenges of incorporating patient preference data into reimbursement and pricing decisions. To reach this goal, 4 polls were conducted, followed by a discussion after each poll.
Figure 1. Panelists (left to right): Esther de Bekker-Grob, Kevin Marsh, Jacoline Bouvy, and Mendwas Dzingina.
Incorporating Patient Preferences in HTA
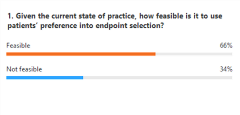
Poll 1: Should patients’ preferences be used to support HTA?
A majority of the participants (88%) voted for the use of patient preferences to support understanding patients’ treatment choices (Figure 2). To the surprise of all 3 panelists, the choice with the second most votes (72%) was the use of patient preferences to estimate utility gains (to inform a cost-utility analysis). Jacoline Bouvy, PhD, Science Policy and Research Programme, National Institute for Health and Care Excellence, London, United Kingdom added that she would like to use patient preferences for endpoint selection, taking into consideration the obvious caveats. Bouvy argued that the use of patient preference data could be used to understand the endpoints that one is targeting, as well as potential misalignment. She indicated that she would be interested in the use of nonhealth benefit (eg, taking a pill once a week vs once a month).
Figure 2. Responses to Poll Question 1: Should patients’ preferences be used to support HTA?
The audience suggested that patient preferences could be included prior to HTA, (eg, FDA approval) to which Bouvy agreed.
Endpoint Selection
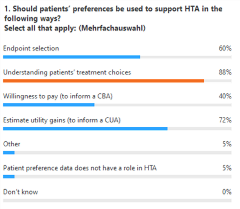
Poll 2: Given the current state of practice, how feasible is it to use patients´ preference in endpoint selection?
Agreeing with the 66% of the audience that it is feasible (Figure 3), Mendwas Dzingina, PhD, Pfizer, London, United Kingdom emphasized the importance of “focusing on what matters to the ones that matter.” Asking patients what outcomes they prefer could help alignment regarding clinical endpoints. The US Food and Drug Administration (FDA) declared the importance of the topic by publishing guidelines on how to incorporate patient preferences right from the start—the endpoint selection.
Figure 3. Responses to Poll Question 2: Given the current state of practice, how feasible is it to use patients´ preference in endpoint selection?
Bouvy added that the feasibility depends on disease, patient population, and practical limitations (eg, orphan diseases).
Patients’ Treatment Choices
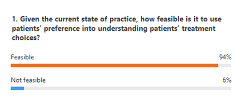
Poll 3: Given the current state of practice, how feasible is it to use patients´ preference in understanding patients´ treatment choices?
In accordance with the audience’s answers of 94% feasibility (Figure 4), Bouvy and the other panelists emphasized the general feasibility in this context. Limitations were brought up by Mendwas Dzingina, PhD, Pfizer, Tadworth, United Kingdom. He stated a few scenarios where the preferences could only be used narrowly (eg, cognitive impairment, children, and end of life). However, the use of surrogate parameters was suggested to derive the data.
Figure 4. Response to Poll Question 3: Given the current state of practice, how feasible is it to use patients´ preference in understanding patients´ treatment choices?
Utility Gains
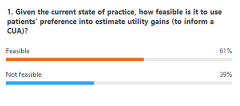
Poll 4: Given the current state of practice, how feasible is it to use patients´ preference in estimating utility gains (to inform a cost-utility analysis)?
While 61% of the audience agreed (Figure 5), Kevin Marsh, PhD, Evidera, Newport Pagell, United Kingdom started the discussion by stating that discrete choice experiments have very different scales than the ones used in HTA right now. Moreover, he assumed missing consistency in the participants’ answers in discrete choice experiment studies (eg, differing value of survival perceived by the patients). Furthermore, the option of evaluating the utility with a discrete choice experiment and transferring it to comparable metrics and thus making it comparable with other values such as survival rate was proposed.
“What is the appropriate role of the patient in health technology assessment?” —Kevin Marsh, PhD
Bouvy pointed out the contradiction to the NICE perspective that health utility should come from the general population and should reflect this very population. However, she mentioned that utility decrements are used to reflect major adverse events, something that could be used as a rule for discrete choice experiments. The audience added: “In theory, all these options are feasible, but not easy, practical, or routinely done currently.”
Figure 5. Response to Poll Question 4: Given the current state of practice, how feasible is it to use patients´ preference in estimating utility gains (to inform a cost-utility analysis)?
Consistency Needed
The role of patient preferences in HTA has not been fully clarified yet. New consistent methodologies need to be established.