“New Deal” for Healthcare Systems: Mission Inspirational, Impossible, or Inevitable?
Aakash Bipin Gandhi, BPharm, Department of Pharmaceutical Health Services Research, University of Maryland, Baltimore, MD, USA; Vasco Pontinha, MPharm, MA, Department of Pharmacotherapy and Health Outcomes, Virginia Commonwealth University School of Pharmacy, Richmond, VA, USA
The first plenary session titled, “’New Deal’ for Healthcare Systems: Mission Inspirational, Impossible, or Inevitable” was kicked off by Paola Testori Coggi (National Technological Cluster on Life Sciences (ALISEI), European Commission, Italian Medicines Agency, Milan, Italy). Coggi laid out pressing questions related to problems that healthcare systems currently face, such as ensuring equitable access to drugs, sustaining innovation for discovery of novel drugs, and challenges faced with reaching a final consensus on defining value-based healthcare.
Warehousing Data to Ensure Efficiency
Up until recently, R&D (research and development) initiatives have appeared to register a high attrition rate. Nevertheless, this trend has inverted, with R&D initiatives becoming increasingly efficient in terms of their translation to relevant and successful projects. Fabio Pammolli, Politecnico di Milano, Milan, emphasized that to ensure this trend of pharmaceutical innovation continues, key challenges must be addressed. These include maintaining the financial sustainability of healthcare systems, especially during current times where a majority of resources have been redirected to address the COVID-19 pandemic.
Further, there is a need for a thorough evaluation and clear communication surrounding any clinical assumptions made through the product life cycle, especially for highly innovative drugs. Pammolli argued that since data involved in the drug development process stem from several sources (including pharmaceutical companies, hospitals, or research institutes) there is a need to integrate and store these in a central warehouse to ensure efficient access and analysis. Pammolli also noted that, “In addition to the challenge of building such a data infrastructure, decision makers must be trained in relevant machine learning and causal econometric modeling techniques that help in result generation to guide evidence-based policy decisions.”
“Not all innovation is valued equally: there is a need to fund today’s patients, as opposed to singly focusing on the benefits for tomorrow’s patients."—Natasha Azzopardi-Muscat, MD, PhD
Unmet Needs Lead to Inequality of Care
Natasha Azzopardi-Muscat, MD, PhD, World Health Organization Europe, Copenhagen, Denmark, provided an interesting perspective on the challenges faced by countries in defining value-based healthcare. “While pharmaceutical innovation yields unparalleled results in improving health outcomes, there are still therapeutic areas with pressing unmet needs.” An example includes problems associated with treating antibiotic resistance. In addition, Azzopardi-Muscat pointed out that, “Not all innovation is valued equally: there is a need to fund today’s patients, as opposed to singly focusing on the benefits for tomorrow’s patients.” Therefore, pharmaceutical innovators and healthcare systems need to agree on how realistic it is to keep funding (all) innovation. With this in mind, Azzopardi-Muscat provided the example of the Oslo Sustainable Development Goals Initiative, which aims to bridge the gap between research and policy and takes a leading role in promoting cross-sectoral partnerships, collaboration, and dialogue between various stakeholders.
Because there are no generics without previous branded [innovative] drugs, the short-term pain of purchasing expensive drugs may very well justify the long-term economic benefit of innovation. —Jack Scannell
Measuring Value for Both Patients and Healthcare Systems
The perspective of the pharmaceutical industry was given by Nathalie Moll, EFPIA, Brussels, Belgium. Moll argued that, “To keep up with the pace of innovation, healthcare systems should implement smart spending measures.” This requires both innovators and policy makers to agree on and develop measures that look at what value means for both the patient and the healthcare system as a whole. In addition, Moll highlighted that there are significant learnings that we should use from the current pandemic such as the development of early detection technologies and tracing systems. Finally, Moll explained how EFPIA is engaging with decision makers so that innovation is not stifled. The organization is publishing a series of best practices on novel pricing and payment methods from all around the world and working towards eliciting the root causes of delays in accessing innovation.
Short-Term Pain Versus Long-Term Benefits
Jack Scannell, JW Scannell Analytics Ltd, University of Edinburgh, Edinburgh, Scotland, discussed how value is actually shared. In short, pharmaceutical companies price their products at a price that markets can bear, regardless of the value measurements used (Figure 1). The healthcare system wishes to use a value measurement that minimizes the cost of the drug, while the pharmaceutical companies want to deploy an all-encompassing value measurement, justifying the high price of drugs. Scannell noted that, “Generic pharmacopeia is the main way consumers capture healthcare value from drugs.” Because there are no generics without previous branded [innovative] drugs, the short-term pain of purchasing expensive drugs may very well justify the long-term economic benefit of innovation. According to EFPIA, high prices alone do not seem to hinder equitable access to drugs. Delays and long waiting times caused by lengthy price and reimbursement negotiations and readiness of healthcare systems seem to be the root causes of access issues.
Figure 1. How much value is created by drugs?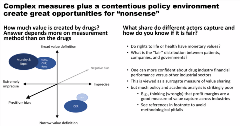
“Innovation is not meaningful if there is no access.”
—Natasha Azzopardi-Muscat, MD, PhD
A Balancing Act
In conclusion, the panelists (Figure 2) agreed on the need for increased cooperation between stakeholders to ensure equitable access to drugs and a need for transparency in methods involved in measuring and defining value. Azzopardi-Muscat pointed out that “innovation is not meaningful if there is no access” and achieving a fair balance between both is not ‘Mission Impossible’ but ‘Mission Inevitable.’"
Figure 2. Session Panelists

The panelists concluded by highlighting the common ground reached on topics discussed during the session: 1) concentrating research in most rewarding disease areas and so that regulators can fine-tune the economic incentives for these diseases; 2) regulators need to engage with innovators to continuously evaluate the clinical meaningfulness of each drug; 3) cooperation between EU-members is critical in order to develop policies that provide equal access to innovative treatments, and finally; 4) the definition of value needs to become more transparent so that the negotiation between payers and innovators yields fair and timely access to innovative therapies.

