Investing in Healthcare Interventions: Finding a Common Threshold
Section Editors: Soraya Azmi, MBBS, MPH, Beigene, USA; Agnes Benedict, MSc, MA, Evidera, Budapest, Hungary
The use of cost-effectiveness thresholds for evaluating health interventions in low- and middle-income countries from 2015 to 2020: a review
Kazibwe J, Gheorghe A, Wilson D, Ruiz F, Chalkidou K, Chi YL
Value Health. 2022;25(3):385–389.
https://www.valueinhealthjournal.com/
When investing in healthcare interventions, decision makers apply multiple criteria,1 including the relative cost-effectiveness of different investment options (ie, the incremental cost-effectiveness ratio [ICER]). The ICER, estimated for various health-effectiveness metrics such as life years gained, quality-adjusted life years gained, or disability-adjusted life years avoided, etc2 is then compared against a cost-effectiveness threshold (CET) and a judgment about the intervention being cost-effective is made. The threshold would generally reflect healthcare budget constraints in the given country.
In low- and middle-income countries (LMICs), the ICER is preferably measured as cost per disability-adjusted life years avoided.3 A CET standard for LMICs of 1 to 3 times the gross domestic product (GDP) per capita was proposed as a rule of thumb by the World Health Organization in 2001.4
In India, with a GDP per capita estimated at about $7000,5 implementing a new healthcare intervention is deemed cost-effective if, for each avoided disability-adjusted life year by the new intervention, society spends less than $21,000 over a given time horizon. In comparison, the threshold in European countries is set between €20,000 and €50,000, compared to the mean GDP of €40,000 of the 27 European Union member states.5
Estimating a threshold based on GDP per capita has long been criticized as being high and not reflecting healthcare budget constraints and opportunity costs of an intervention in LMICs.6 In this context, the authors set out to investigate the usage of thresholds based on GDP per capita in LMIC studies in recent years and the relationship between recommendations by the authors and the threshold applied.
The authors searched interventions and studies in the Global Health Cost-Effectiveness Analysis Registry7 from January 2015 to January 2020, selecting LMICs studies using cost per disability-adjusted life year as an ICER metric and extracted the type of threshold used and the conclusion on the cost-effectiveness of interventions.
Overall, 713 healthcare interventions reported in 230 studies were identified, most of which were conducted in sub-Saharan Africa and South Asia. About half of the 230 selected studies compared preventive healthcare interventions: 26% for immunization, 15% for screening, and 7% other public health. Although the proportion of prevention in developed countries is unknown, assessment of technologies to prevent diseases seems to represent a significant amount of the research in the cost-effectiveness fields for LMICs. This is consistent with the assumption that LMIC societies have a propensity to invest in healthcare interventions that prevent the congestion of healthcare resources such as nurses, physicians, hospital beds, material and medication stocks/supply, etc. Therefore, opportunity costs are also considered when defining thresholds for cost-effectiveness as highlighted by the authors.
Thresholds identified in the paper were classified into 3 categories: (1) GDP-based thresholds, which equal to 1 to 3 times GDP per capita in the country, (2) opportunity costs thresholds, which equal to 0.5 GDP per capita, justified as being an appropriate measure of opportunity costs8,9 and, (3) willingness-to-pay thresholds, which represent the less explicit yet more comprehensive category of society’s valuation of healthcare benefits.
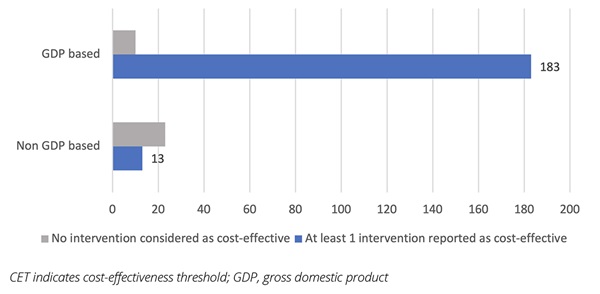
Of the 230 identified studies, 80% use the World Health Organization’s GDP based threshold, as illustrated in Figure 1. Besides, as illustrated in Figure 2, 94% of the studies using a GDP-based CET (ie, 1 to 3 times the GDP per capita as threshold) report at least 1 healthcare intervention as being cost-effective, versus 36.1% of the studies using a non-GDP–base threshold (ie, opportunity cost, CET, or other).
Figure 1. Distribution of studies according to the type of CET.
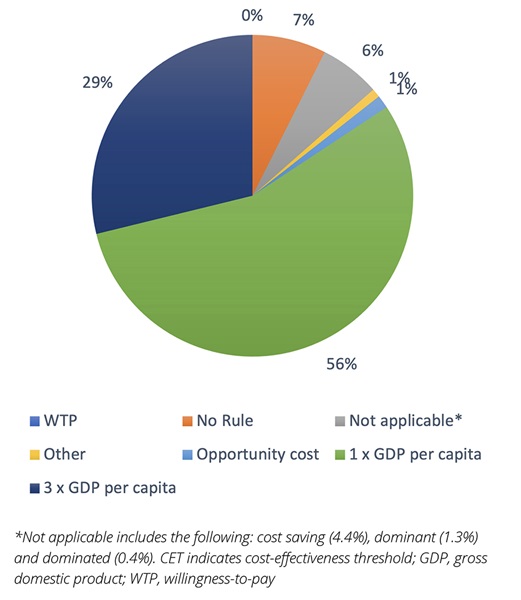
The 1-3 GDP per capita as a CET threshold to conclude the cost-effectiveness of healthcare interventions is still widely in use in published LMICs studies, despite previous criticisms about its appropriateness and warnings that application of such thresholds cannot appropriately prioritize healthcare interventions using cost-effectiveness in LMICs.
Figure 2. Number of studies by CET type and conclusions on cost-effectiveness.
Clearly, publications do not reflect the actual reimbursement/adoption decisions in these countries and the role of cost-effectiveness analyses may vary in healthcare decision making. However, further research would be required to identify the appropriate thresholds for each LMIC to ensure the credibility of health economic research for these geographies, and hence their usefulness for decision making. Readers of this article will receive an overview of previous literature on this topic of thresholds in LMICs, the cost-effectiveness analyses published for these countries and will understand why it is important to carefully consider the threshold to be used to make conclusions about cost-effectiveness of therapies, instead of automatically applying previously used thresholds.
References
1. Mühlbacher AC, Kaczynski A. Making good decisions in healthcare with multi-criteria decision analysis: the use, current research and future development of MCDA. Appl Health Econ Health Policy. 2016;14(1):29-40.
2. Gold MR, Stevenson D, Fryback DG. HALYS and QALYS and DALYS, oh my: similarities and differences in summary measures of population health. Annu Rev Public Health. 2002;23:115-34.
3. Augustovski F, Colantonio LD, Galante J, et al. Measuring the benefits of healthcare: DALYs and QALYs–does the choice of measure matter? A case study of two preventive Interventions. Int J Health Policy Manag. 2018;7(2):120-136.
4. World Health Organization. Published 2001. Accessed March 8, 2022. Macroeconomics and health: investing in health for economic development. Report of the Commission on Macroeconomics and Health. http://apps.who.
5. Organisation for Economic Co-Operation and Development. Stat. Level of GDP per capita and productivity. Accessed March 8, 2022.
6. Robinson LA, Hammitt JK, Chang AY, Resch S. Understanding and improving the one and three times GDP per capita cost-effectiveness thresholds. Health Policy Plan. 2017;32(1):141-145.
7. Center for the Evaluation of Value and Risk in Health. Global Health Cost Effectiveness Registry. Accessed March 8, 2022.
8. Woods B, Revill P, Sculpher M, Claxton K. Country-level cost-effectiveness thresholds: initial estimates and the need for further research. Value Health. 2016;19(8):929-935.
9. Ochalek J, Lomas J, Claxton K. Estimating health opportunity costs in low-income and middle-income countries: a novel approach and evidence from cross-country data. BMJ Global Health. 2018;3(6):e000964.