Beyond Cost-Effectiveness: Defining and Mapping Out Innovation at NICE

Health technology assessment (HTA) is facing one of the biggest turning points in its history. COVID-19 stressed healthcare systems almost to the breaking point while creating a demand for quick assessment for new therapies and treatment protocols. Scientific advances in such areas as gene therapy have created new drugs and artificial intelligence has sped up the process of drug development.
As the tidal wave of potential new therapies from development pipelines threatens to crash down, HTA organizations face major challenges. These bodies, short on resources, will have to figure out the best ways to evaluate these new technologies for the benefit of all stakeholders. They are caught in the age-old paradox of “fast and good, but not cheap,” “fast and cheap, but not good,” and “cheap and good, but not fast.” While speed is called for, HTA agencies must at the same time balance patient need to access new technologies with ensuring the independence and scientific and methodological rigor of the HTA process.
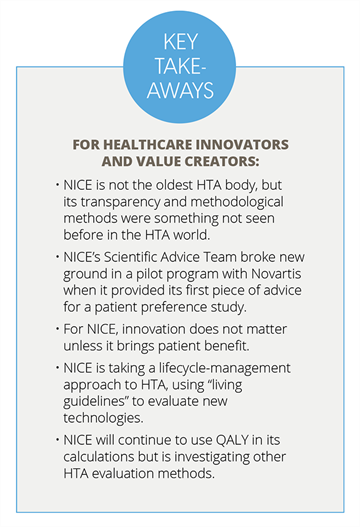
The UK’s National Institute for Health and Care Excellence (NICE), realizing these challenges, has created a 5-year strategy for 2021 to 2026. As one of the most-experienced and recognized HTA bodies in the world, the agency has prided itself on being rooted in innovation and its strategy has 4 pillars that reflect that legacy. The agency wants to: (1) provide rapid, robust technology evaluation; (2) create dynamic, living guideline recommendations; (3) make sure guidelines are effectively adopted and used by NICE’s strategic partners; and (4) drive progress in data, research, and science.
The new strategy is intended to help the life sciences industry seeking market access for their technologies, provide guideline recommendations for healthcare providers and commissioners that incorporate up-to-date evidence and data, and give patients improved access to healthcare technologies as well as new ways of engaging and using patient and public opinion to inform the evidence base for guidance development.
Additionally, international partners will see greater collaboration and sharing of NICE’s expertise and knowledge through NICE International, a not-for-profit advisory service aimed at health organizations, ministries, and government agencies.
Jens Grueger, Director and Partner, Boston Consulting Group, readily concedes that NICE is more known for being a hawk when it comes to drug and medical pricing than for innovative techniques in considering how therapies are approved and priced. But from its very beginning, the organization has been an innovator.
“NICE has been the agency that has given the payers teeth, but in a way that was hard for others to criticize it because they had a very strong methodological foundation,” he says. “And they published their methods guidelines, they were extremely transparent. That was very different from what we had seen before. Nobody had pledged so much transparency about their initial assessments, how they were then holding public meetings to look at these things. NICE was always punching above its weight in terms of the methodological foundation, the transparency, and the visibility of what they were doing.”
Another way in which NICE has been an innovator is its openness in engaging with healthcare companies, particularly through its Scientific Advice Team. The team is a fee-based advisory service for pharmaceutical, medical device, and other healthcare technology developers. When the team was launched in 2007, Grueger says patient groups and academia expressed fear that NICE would develop biases. But that wasn’t the case. “Sir Andrew Dillon’s, the founding and first chief executive of NICE, response was, ‘The only way to deal with bias is to have all the biases sat around the table,’” Grueger says.
“The thing that matters to NICE about innovation is being able to demonstrate that that brings patient benefit, and that is still absolutely core and fundamental to what we do in our evaluations.” — Gillian Leng
While fending off accusations of bias, the Scientific Advisory Team has engaged in innovation. In 2019, the team (in a pilot program with Novartis) provided its first piece of advice on the design of a patient preference study in chronic obstructive pulmonary disease. “We see this engagement during the project design phase as a positive step, helping to ensure the results serve the interests of the different stakeholders: industry, NICE, and the patient community,” said Nigel Cook, Head of Decision Support and Insights, Global Patient Access, Novartis.
At the time Grueger was working for Novartis, so he saw firsthand how the pilot program worked. Until that point, the pharmaceutical industry was struggling with NICE’s rejections of results from patient preference studies. “I think the industry was getting frustrated that whatever data were produced, whatever models were produced, NICE was always finding something wrong with fixed models,” Grueger says. He believes that as a result of the pilot program other countries have learned that having this kind of scientific advice available to the industry is important.
NICE and the Definition of Innovation
Gillian Leng, NICE’s Chief Executive, says defining innovation generally is difficult, because “the word innovation is used in all sorts of different ways. And there’s a general way that people often describe innovation as shorthand for change and ongoing development and improvement.”
But NICE has never been interested in that shorthand definition. Back in 2009, Professor Sir Ian Kennedy, in his “Appraising the Value of Innovation and Other Benefits: A Short Study for NICE,” came up with a much more concrete description, Leng says. “The thing that matters to NICE about innovation is being able to demonstrate that that brings patient benefit,” she states. “And that is still absolutely core and fundamental to what we do in our evaluations. Because you could have a hugely innovative new molecule that nobody ever has created, but there’s no point in those innovations—unless they bring patient benefit.”
According to Meindert Boysen, PharmD, MSc, Director, Centre for Health Technology Evaluation, NICE, innovation is about a new solution for something that has a high demand or an unmet need. “Just because something is new doesn’t really matter,” Boysen says. “It’s relative to what we currently have.”
For NICE, employing innovation in the way it conducts its HTA evaluations is important. But Boysen believes that the organization, through its evidence-based approach, has shaped the value of innovation.
NICE and Future Innovation
As new therapies are generated with new technologies, particularly cancer therapies and digital therapies for mental health issues, NICE is faced with the prospect of making decisions about clinical and cost-effectiveness without a lot of data to consider. “We have to deal with an ever-greater uncertainty around new technology,” Boysen says. “We don’t really have the evidence, but people want the answer now. You have two options, either you say, ‘Well, I’m not giving you the answer,’ and you wait. But that’s really not the one that people support. Or you can give an answer, but with a real clear management plan around it.”
As part of the organization’s new 5-year strategy—embedding those technologies into living guidelines that can position technologies in the pathway of care—NICE will be setting up standing committees that cover topics such as mental health, cardiovascular disease, and cancer. “They can keep track of that more living environment and can see where things might now have a competitor, or whether they might now be less important in a pathway,” Leng says.
For these living guidelines to work, NICE will have to collaborate—connecting regulators, commissioners, payers, patient groups, and pharmaceutical and medical device companies. “We are absolutely the type of organization that can bring a lot of people together around a plan for an early value assessment, with a contingent or managed access approach to introduction, that then leads into a living guideline when the product is linked into a pathway,” Boysen says. “It’s a life cycle approach for health technology management.”
“We don’t really have the evidence, but people want the answer now. You have two options, either you say, ‘Well, I’m not giving you the answer,’ and you wait. But that’s really not the one that people support. Or you can give an answer, but with a real clear management plan around it.” — Meindert Boysen, PharmD, MSc
While NICE will continue to evolve its processes and be open to looking at other ways of evaluating new technologies, the quality-adjusted life year (QALY) is sticking around—at least for now. “We are investing ourselves in a research project called ‘Beyond the QALY,’ so we’re open to doing that,” Boysen says. “But we position ourselves in a relatively closed system in which we consider the kind of budget constraints of our healthcare system, combined with a specific environment of liaising with commissioners and regulators, which makes the tradeoffs that we have to make best express to the QALY because the QALY reflects a unitary measure that makes it relatively simple for us to make those tradeoffs.”
At the time when NICE was established, the QALY was deemed the best way to give evaluators a level playing field in order to compare one thing to another. “It has stood us in good stead,” Leng says. “It’s not simply a technical calculation, it is important that we remember the other factors that committees look at, too. And I think it’s really important that we do look for new ways, but that we do all of that cautiously because it stood us in good stead for 20-odd years. And it would be foolish to suddenly put that all to bed and start doing something else. It’s very much going to be careful evolution.”
HTA, Innovation, and ISPOR
Leng, Boysen, and Grueger spoke about NICE’s strategy for future innovation in July, at ISPOR’s third installment in the Signal series. ISPOR started the Signal program to bring a broader understanding of innovation (beyond product innovation), with the goal of putting these issues front and center for the health economics and outcomes research (HEOR) community. Each episode in a series is a self-contained installment and not dependent on the previous episodes; however, all of them are connected by an intent to look at the concept of innovation and experience with it from different groups of healthcare stakeholders, building foresight into how these innovations might impact healthcare decision making in the next decade.
The first Signal program, “Next Gen Innovation: ‘How To’ From the US Department of Veterans Affairs,” highlighted how the US Department of Veterans Affairs’ ecosystem has emerged as a model for supporting the entire life cycle of innovation in a large and highly complex integrated health system. ISPOR’s second Signal series event, “From Price Determining Value to Value Determining Price: It’s About Strategy at a System Level,” looked at how to bring systems-level thinking to healthcare and how the pharmaceutical industry, payers, and HEOR experts can work together in a new system for commercial strategy. ISPOR recently held its fourth Signal event, “Venture Capital Investment: Upstream Decision Making on Value in Healthcare,” which examined how innovation in healthcare—from therapies to research on the best care protocols—is funded before concrete solutions come to the market, and how that paradigm can change.
The Next Signal Program
The next Signal episode, “The New Science of Cause and Effect: Causal Revolution Applied,” is scheduled for January 25, 2022. The event features Judea Pearl, professor of computer science and director of the Cognitive Systems Laboratory, Samueli School of Engineering, UCLA, Los Angeles, CA, USA, a world-renowned computer scientist and philosopher. He is known for his world-leading work on artificial intelligence and the development of Bayesian networks, as well as his theory of causal and counterfactual inference. Dr Pearl will speak on how causal models interact with data and work in scientific applications today, spanning the subjects of selection bias, personalized treatment effect, fusion of data from several sources (observational and experimental studies), and causality in observational studies. The conversation with Dr Pearl will focus on the challenges and opportunities modern computing tools will offer to HEOR research. To register for ISPOR’s next Signal episode, click here.
For more information and to register: www.ispor.org/signal

