Building Cost-Effectiveness Thresholds for the Future
Dimitrios Kourouklis, PhD, Chris Sampson, PhD, Mikel Berdud, PhD, Chris Skedgel, PhD, Office of Health Economics, London, England, United Kingdom
A primer on thresholds
Novel health technologies are routinely both cost-increasing and health improving. Researchers and policy makers have used cost-effectiveness thresholds (CETs) to determine whether a technology’s health benefits are worth the additional cost. Simply put, a CET represents the maximum price per quality-adjusted life year (QALY) at which policy makers would usually judge a technology to be a worthwhile investment. The use of CETs in policy varies across countries and healthcare systems. CETs may be specified explicitly (as in the case of England or of ICER in the United States) or implicitly (as in the case of Australia or Canada).1
Historically, 2 approaches to identifying a CET have been discussed.2 One approach relies on the identification of society’s willingness to pay (WTP) for a QALY (sometimes called a “demand-side” approach). The other relies on estimating the opportunity cost of current expenditure on healthcare, usually in recognition of a fixed budget (sometimes called a “supply side” approach). The opportunity cost approach has been the subject of numerous empirical analyses in recent years. It represents the intuitive notion that, without an excess budget to spend, we should only invest in a technology if we can disinvest in something less cost-effective, thereby increasing overall health gain.3,4 Where a CET is not specified (explicitly) in policy, decisions may be informed by past allocation decisions or decisions in other countries.5 This approach may indicate an implicit threshold but may undermine transparency and consistency in decision making.
"Researchers and policy makers have used cost-effectiveness thresholds to determine whether a technology’s health benefits are worth the additional cost."
More recently, research on CETs has moved toward the development of new theoretical frameworks, based on demand and supply models for healthcare technologies (confusingly, this is distinct from the demand-side and supply-side approaches mentioned earlier). These models seek to facilitate maximization of the total value created by investment in new technologies. This is known as the economic surplus (the sum of consumers’ and producers’ surplus) and the models focus on the distribution of this surplus between healthcare providers, patients, and the life sciences industry.6 In the context of these models, numerous factors may influence the demand and supply of health technologies (including pharmaceuticals, medical devices, and nondrug interventions), such as the distribution of bargaining power and the nature and dynamics of research and development (R&D) costs.7
In this article, we consider these policy-focused research developments and review relevant literature to explore what factors might be used to determine CETs in future.
Connecting evidence to policy
One of the first studies to estimate a supply-side CET was conducted by Claxton et al (2015) in the context of the English National Health Service (NHS).8 That study sought to identify the impact of expenditure on health outcomes and concluded that the current allocation of resources produced QALYs at the cost of around £12,936. This estimate was substantially lower than the threshold used by the National Institute for Health and Care Excellence (NICE) of £20,000-£30,000 per QALY. However, the central estimate was conditional on numerous assumptions—some of which faced criticism9—and different assumptions would lead to different estimates. In 2019, the Voluntary Scheme for Branded Medicines Pricing and Access, agreed between the pharmaceutical industry and the government, maintained NICE’s current threshold of £20,000-£30,000 per QALY.10
Similar studies have been conducted and similar policy-making tales can be told for Spain,11 Australia,12 and a growing number of other countries.13 Most countries do not make use of explicit CETs in policy, and where CETs are used, they are not clearly based on evidence.1 Researchers should consider why the empirical evidence generated to date has not been used to to inform policy.
The evidence generated from these studies examines the impact of current health expenditure on health outcomes, inferring the value of new technologies from the productivity of prevailing care. This is a notoriously difficult thing to estimate with confidence due to the two-way relationship between spending and outcomes, the limited availability of data, and a variety of other technical challenges. Furthermore, these opportunity cost estimates only provide part of the resource allocation puzzle. By broadening the scope of CET estimation (beyond estimates of productivity and informed by various determinants of supply and demand), researchers may be able to provide policy makers with a more complete picture. Currently, there is limited scope for evidence to inform policy on CETs. In the future, a more comprehensive approach may prove successful.
Taking stock of the possibilities
Expanding the scope of CET identification raises the inevitable question: what factors should be considered? Researchers—particularly economists—have recommended numerous factors when considering CETs and pricing policies. To date, nobody has conducted a thorough assessment of these factors.
We conducted a literature review to identify papers in which researchers have modeled—or otherwise proposed—the inclusion of different factors in the identification of a CET. Our objective was to generate a list of candidate factors for inclusion in a framework to identify a CET using models of demand and supply. We sought to classify these factors according to their characteristics in order to guide future research.
Our review identified 40 unique factors that have been discussed in the literature. We identified 22 demand-side, 5 supply-side, and 13 market factors—all summarized in Figure 1. The relationship between factors and the CET could also be classified as static when their whole impact can be consistently estimated at a point in time, or as dynamic when the size and/or sense of their impact show important dependencies over the life cycle of a product.
Figure 1. Identified factors
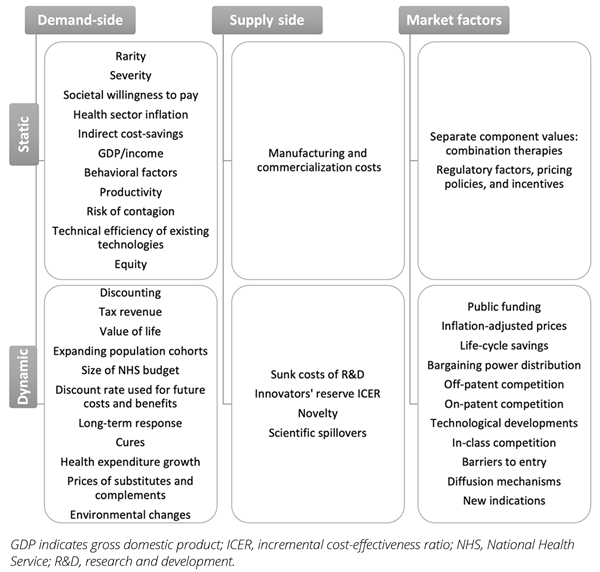
Demand-side factors are those that determine the level of demand for healthcare,
including factors such as hyperbolic discount rates, budget mechanisms, tax revenue, and population growth. Supply-side factors determine decisions by manufacturers about whether to enter the market and their decisions about the level of R&D investment that determines future supply of new health technologies. These factors include the costs of R&D and innovators’ reserve incremental cost-effectiveness ratios (ICERs)—the minimum ICER at which innovators will keep investing in R&D. Market factors may influence supply and demand and their interaction. These include factors such as inflation, competition, bargaining power distribution, and regulatory conditions.
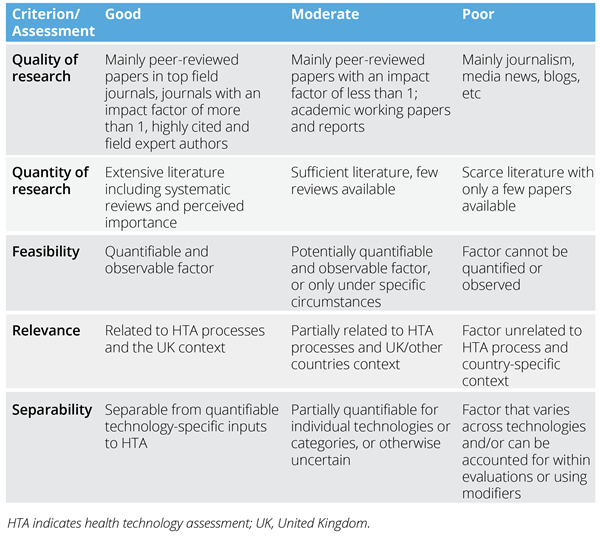
It may be more productive for research to pursue some factors over others; some factors may have been extensively researched while others may simply be ideas recorded in print. We assessed each factor according to its satisfaction of the criteria presented in Table 1 and discussed our findings with an expert advisory group comprising academics and industry representatives.
Table 1. Factor assessment criteria
Based on the subjective assessment and meetings with the expert advisory group, we prioritized and short-listed the following factors as those with greatest potential to play a practical role in the specification of a new framework to identify CETs:
1. Opportunity cost and displacement
2. Budget changes and flexibility
3. Nominal drug prices and inflation
4. Market regulation and competition
5. Bargaining power distribution
6. Elasticity of response of innovators
A substantial body of literature is available for each of these factors and future work should explore the feasibility of incorporating each of these into the identification of a threshold. For instance, it may be possible to establish—in theory and evidence—the extent to which a higher budget (all else equal) corresponds to a higher CET.14
A complex picture
Our literature review uncovered some challenges relating to the appropriate definition of CETs, assumptions underlying each factor, and data availability. In particular, researchers often conflate price and value by regarding CETs as an implicit price-setting mechanism (ie, the notion of manufacturers “pricing to the threshold”). We believe it is important to disentangle these elements: the ICER should be interpreted as the price per unit of effect, while thresholds should be used to guide decision makers on the acceptability of that price, in conjunction with other criteria and value judgments.
More broadly, it is essential to distinguish the different mechanisms for decision making and the various inputs to technology assessment and reimbursement processes. Each of the factors that has been proposed to determine CETs or optimal prices may be most appropriately accounted for via one of several mechanisms. Some of the key mechanisms that are relevant to the factors that we have identified are (i) inclusion within an economic evaluation, (ii) adoption as a quantitative modifier, and (iii) qualitative consideration within an appraisal.
Health economic evaluations should account for all factors that affect the costs and outcomes associated with a specific technology. These will influence the technologies, ICER (which can then be judged against a CET). Modifiers indicate differences in the value of outcomes across different groups of technologies. They are generally used to address equity concerns and should be used to weight QALYs (rather than to identify product- or condition-specific thresholds per se). The appraisal process should incorporate the available quantitative, qualitative, and deliberative input to the decision and is an important mechanism for considering those factors that cannot be easily represented in evidence.
Once the most appropriate factors to consider in the estimation of a CET have been identified, and factors more appropriately considered as part of the ICER have been excluded, data availability and gaps in the research pose further challenges. Researchers must consider what is feasible in different settings.
The way forward
Research on cost-effectiveness thresholds has developed substantially in recent years and there are signs that it is shifting in a new direction. Researchers are right to look beyond the relationship between expenditure and outcomes in healthcare to understand CETs. Our research highlights a vast number of factors that could—in principle—be considered in the identification of a CET.
"It is imperative for researchers and policy makers to adopt a holistic view in the identification and use of cost-effectiveness thresholds and, more broadly, the allocation of healthcare resources."
The adoption of evidence-based policy in defining CETs—whether in terms of opportunity cost or societal willingness to pay—is a worthy objective that could ultimately benefit the health of the population by facilitating a more efficient, health-maximising allocation of resources in healthcare. However, the factors that we have identified paint a complex picture. A cost-effectiveness threshold cannot be adopted as a catch-all value assessment tool. Many factors that determine optimal prices and the relative value of technologies should be incorporated via mechanisms other than a CET.
In navigating this complex landscape, the duty falls as much to policy makers as to researchers. Policy makers should clearly specify the scope and purpose of CETs, as distinct from other mechanisms in the decision-making process. Researchers should explore data sources and develop new methods to incorporate appropriate factors in identifying a CET. It is for the common good to develop a robust framework for the determination of CETs that can support resource allocation while accounting for all relevant factors that may influence current and future population health. It is imperative for researchers and policy makers to adopt a holistic view in the identification and use of cost-effectiveness thresholds and, more broadly, the allocation of healthcare resources. New frameworks and approaches should be considered in countries where explicit thresholds are specified, as well as contexts with less formalized resource allocation processes.
Funding/Support:
This work was funded by the Association of the British Pharmaceutical Industry (ABPI). The views presented do not represent those of the ABPI.
References
1. Zhang K, Garau M. International Cost-Effectiveness Thresholds and Modifiers for HTA Decision Making.; 2020. Accessed February 4, 2022. https://www.ohe.org/publications/international-cost-effectiveness-thresholds-and-modifiers-hta-decision-making.
2. Vallejo-Torres L, García-Lorenzo B, Castilla I, et al. On the estimation of the cost-effectiveness threshold: why, what, how? Value Health. 2016;19(5):558-566. doi:10.1016/j.jval.2016.02.020
3. Pekarsky BA. The “New Drug Reimbursement” Game. In: The New Drug Reimbursement Game. Springer; 2015:127-162.
4. Thokala P, Ochalek J, Leech AA, Tong T. Cost-effectiveness thresholds: the past, the present and the future. PharmacoEconomics. 2018;36(5):509-522. doi:10.1007/s40273-017-0606-1
5. Eichler HG, Kong SX, Gerth WC, Mavros P, Jönsson B. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost-effectiveness thresholds expected to emerge? Value Health. 2004;7(5):518-528. doi:10.1111/j.1524-4733.2004.75003.x
6. Patented Medicine Prices Review Board. Working Group to Inform the PMPRB Steering Committee on Modernization of Price Review Process Guidelines - Final Report. 2019. Accessed February 2, 2022. http://pmprb-cepmb.gc.ca
7. Berdud M, Ferraro J, Towse A. A Bargaining Approach: A Theory on ICER Pricing and Optimal Level of Cost-Effectiveness Threshold. Office of Health Economics; 2020. Accessed July 5, 2021. https://www.ohe.org/publications/bargaining-approach-theory-icer-pricing-and-optimal-level-cost-effectiveness-threshold
8. Claxton K, Martin S, Soares M, et al. Methods for the estimation of the National Institute for Health and Care Excellence cost-effectiveness threshold. Health Technol Assess. 2015;19(14):1-503, v-vi. doi:20150217140715559
9. Barnsley P, Towse A, Karlsberg Schaffer S, Sussex J. Critique of CHE Research Paper 81: Methods for the Estimation of the NICE Cost Effectiveness Threshold. 2013. Accessed July 5, 2021. https://www.ohe.org/publications/critique-che-research-paper-81-methods-estimation-nice-cost-effectiveness-threshold
10. DHSC. The 2019 Voluntary Scheme for Branded Medicines Pricing and Access. 2018. Accessed June 28, 2022. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/761834/voluntary-scheme-for-branded-medicines-pricing-and-access-chapters-and-glossary.pdf
11. Vallejo-Torres L, García-Lorenzo B, Serrano-Aguilar P. Estimating a cost-effectiveness threshold for the Spanish NHS. Health Econ. 2018;27(4):746-761. doi:10.1002/hec.3633
12. Edney LC, Haji Ali Afzali H, Cheng TC, Karnon J. Estimating the reference incremental cost-effectiveness ratio for the Australian health system. Pharmacoeconomics. 2018;36(2):239-252. doi:10.1007/s40273-017-0585-2
13. Edney LC, Lomas J, Karnon J, et al. Empirical estimates of the marginal cost of health produced by a healthcare system: methodological considerations from country-level estimates. PharmacoEconomics. 2022;40(1):31-43. doi:10.1007/s40273-021-01087-6
14. Brouwer W, van Baal P, van Exel J, Versteegh M. When is it too expensive? Cost-effectiveness thresholds and health care decision-making. Eur J Health Econ. 2019;20(2):175-180. doi:10.1007/s10198-018-1000-4