Characterizing Telehealth Utilization From Administrative Claims in the United States Using a Standardized Definition
Ramya Avula, MS, Michael Grabner, PhD, Biruk Eshete, MS, Carelon Research, Wilmington, DE, USA; Eric Stanek, PharmD, Elevance Health, Indianapolis, IN, USA; Vincent Willey, PharmD, Carelon Research, Wilmington, DE, USA
Telehealth and the COVID-19 pandemic
Before the COVID-19 pandemic response disrupted the healthcare system, the vast majority of patients in the United States had never used telehealth (TH) services.1,2 The onset of the pandemic led to large decreases in patients’ ability and willingness to participate in in-person care, driven by healthcare delivery policy changes as well as individual patient preferences. Both public and private payers expanded their coverage and reimbursement for TH services starting in March 2020 to encourage continuous access to the healthcare system. As a result, the United States experienced a large increase in TH use in both Medicare and commercially insured populations.3-5 While TH supplied critical access to the healthcare system during the height of the pandemic, this increased accessibility did not compensate for the reduced utilization of healthcare overall, and had strong disparities along age, region, and other domains.6 Research is needed to evaluate the effectiveness and safety of medical care delivered via TH and assess how it can best be implemented within the current healthcare delivery framework.7
"While telehealth supplied critical access to the healthcare system during the height of the pandemic, this increased accessibility did not compensate for the reduced utilization of healthcare overall, and had strong disparities along age, region, and other domains."
Administrative claims are an important source of real-world data that can be used for TH-focused research. However, a wide variety of TH definitions and identification algorithms are being used by different entities and cross-study comparisons are difficult.8-10 In this article, we propose a standardized claims-based definition of TH in the outpatient setting and use it to investigate trends in TH utilization in a large US commercially insured and Medicare Advantage/Supplement population.
"During the study period we identified approximately 75 million outpatient telehealth claims associated with approximately 12 million unique health plan members."
Algorithm definition
We conducted a retrospective study using medical claims from the Healthcare Integrated Research Database (HIRD®) between January 1, 2006, and December 31, 2022. The HIRD contains longitudinal claims and eligibility data from a large national US health insurer offering health plans across many geographically diverse states and includes members with either commercial or Medicare Advantage/Supplement insurance representative of all 50 states. We used a limited dataset (information that excludes direct individual identifiers) in compliance with the Health Insurance Portability and Accountability Act Privacy Rule.
All analyses were descriptive. We evaluated the utilization of TH in an outpatient setting over time using a combination of place of service codes, Current Procedural Terminology (CPT) codes, CPT modifiers, Healthcare Common Procedure Coding System (HCPCS) codes, revenue codes, and certain tax identification numbers (TaxIDs) from known TH providers. The presence of at least one of the below codes was used to classify a claim as TH:
• Centers for Medicare & Medicaid Services (CMS) Place of Service11 - ‘02’ or ‘10’
• CPT and HCPCS codes - ‘98966’*, ‘98967’*, ‘98968’*, ‘98969’, ‘98970’, ‘98971’, ‘98972’, ‘99367’, ‘99368’, ‘99371’, ‘99372’, ‘99373’, ‘99421’, ‘99422’, ‘99423’, ‘99441’*, ‘99442’*, ‘99443’*, ‘99444’, ‘99446’, ‘99447’, ‘99448’, ‘99449’, ‘99451’, ‘99452’, ‘99453’, ‘99454’, ‘99457’, ‘99458’, ‘0188T’, ‘G0406’, ‘G0407’, ‘G0408’, ‘G0425’, ‘G0426’, ‘G0427’, ‘G0459’, ‘G0508’, ‘G0509’, ‘G2010’, ‘G2012’, ‘G2061’, ‘G2062’, ‘Q3014’, ‘T1014’, ‘S0320’, ‘G0071’, ‘G0181’, ‘G0182’, ‘0488T’, ‘0074T’, ‘0488T’, ‘0206T’, ‘93050’, ‘96120’, ‘96146’, ‘G2250’, ‘G2251’, ‘G2252’, ‘G0425’, ‘G0426’, ‘G0427’
• CPT and HCPCS modifiers - ‘GT,’ ’GQ,’ ’G0,’ ’95,’ ’93’
• Revenue Codes - Starting with ‘078’
• TaxIDs - [Confidential]
A subset of codes (bolded & starred) was used to identify audio-only TH visits. CMS enacted a policy change effective March 2020 that introduced coverage for telephone evaluation and management services.12
Algorithm application
During the study period we identified approximately 75 million outpatient TH claims (fully adjudicated and paid) associated with approximately 12 million unique health plan members. Of the associated members, 88% were commercially insured, 6% had Medicare Advantage plans, and 4% had Medicare Supplement plans (other Medicare plans accounted for the rest). Approximately 97% of all TH claims since 2006 occurred in 2020 (33%), 2021 (33%), and 2022 (31%). In 2019 to 2022, the annual share of outpatient claims designated as TH was 0.1%/4.8%/4.1%/3.8%, respectively. Since the vast majority of TH claims occurred from 2020 onward, the analyses presented focus on that time period.
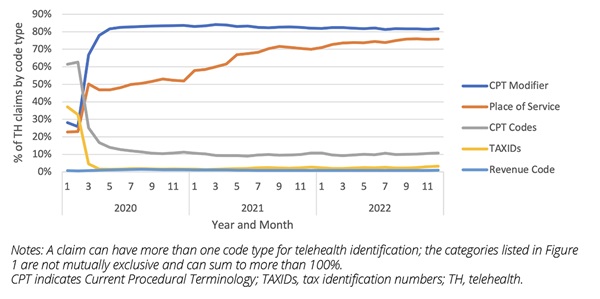
The majority of claims were identified as TH through use of either CPT modifiers or place of service codes (these are not mutually exclusive; a claim can be flagged as TH through one or more codes). The share of claims with a designated TH place of service code increased from less than 50% to more than 70% since March 2020. An additional place of service code (“10”) was authorized by CMS starting January 2022, and we have observed utilization of this code over the course of that year.13 Except for a few months, TH claims identified via TaxIDs contributed a negligible amount of TH utilization (Figure 1).
Figure 1. Distribution of telehealth claims by code type
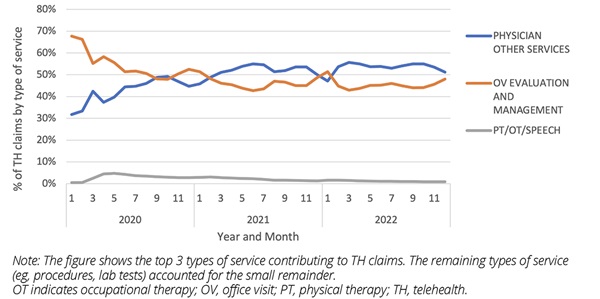
Outpatient services are classified using a modification of the Berenson-Eggers Type of Service (BETOS) categorization involving 10 mutually exclusive categories.14 The distribution of TH claims across BETOS categories changed during the first few months of the pandemic (due to new coding practices having to evolve), with almost all falling under Office Visits (Evaluation & Management) and Physician Other Services (e.g., CPT codes associated with hospital and home visits; specialist visits) since that point (Figure 2).
Figure 2. Distribution of telehealth claims by type of service
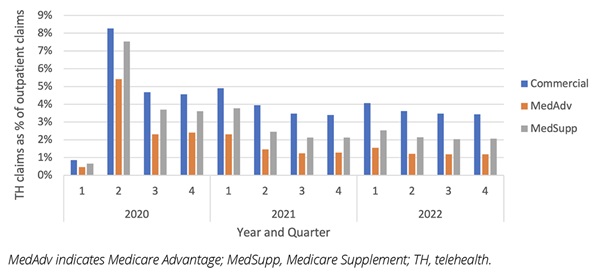
Insurance type affected TH utilization, which was higher among commercially insured compared to Medicare Advantage members (Figure 3). This analysis also indicates that TH utilization peaked at around 8% of all outpatient claims in the first half of 2020, exhibits a seasonal pattern, and remains at 2% to 4% through 2022 in this population. National reports (through August 2021) show similar trends in overall and age-stratified utilization.1
Figure 3. Prevalence of telehealth use by insurance type
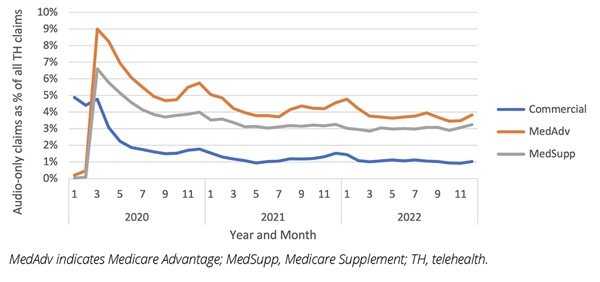
Approximately 2% of TH claims were for audio-only visits based on submitted codes. Distributions by insurance type in 2020 through 2022 are shown in Figure 4, indicating highest utilization in the Medicare Advantage population.
Figure 4. Prevalence of audio-only telehealth by insurance type
Limitations
Certain limitations apply to our analysis. While we created and refined the TH definition in collaboration with a large national payer, we did not conduct benchmarking against external data (e.g., medical records). All findings should be interpreted considering the caveats commonly associated with administrative claims database analyses, including potential coding errors and incomplete data. Lastly, our analysis was conducted in a US population with commercial and Medicare Advantage/Supplement health insurance coverage, which could limit the generalizability of the results to those with other types of insurance such as traditional fee-for-service Medicare or Medicaid, none, or a population outside the United States.
Conclusions
We created a standardized definition to identify outpatient TH using claims data, accounting for coding practices through the end of 2022. Consistent with prior reports, TH utilization increased substantially following onset of the COVID-19 pandemic in conjunction with increased coverage and reimbursement for the service. Utilization then decreased but remains noticeably higher than before March 2020. Incorporation of TH utilization via a broad standardized definition is an essential tool for all health economic and outcomes research studies evaluating time periods from 2020 and beyond.
References
1. Lo J, Rae M, Amin K, Cox C. Outpatient Telehealth Use Soared Early in the COVID-19 Pandemic but has Since Receded. Peterson-KFF Health System Tracker. Access & Affordability Web site. Published 2022. Updated February 10, 2022. Accessed March 27, 2023. https://www.healthsystemtracker.org/brief/outpatient-telehealth-use-soared-early-in-the-covid-19-pandemic-but-has-since-receded
2. Malani P, Kullgren J, Solway E, Buis L, Singer D, Kirch M. National Poll on Healthy Aging: Telehealth Use Among Older Adults Before and During COVID-19. University of Michigan. Published 2020. Accessed March 27, 2023. https://deepblue.lib.umich.edu/bitstream/handle/2027.42/156253/0212_NPHA-telehealth-report-FINAL-08142020-v6-handle.pdf?sequence=4&isAllowed=y
3. US Department of Health and Human Services Office of Inspector General. Telehealth Was Critical for Providing Services to Medicare Beneficiaries During the First Year of the COVID-19 Pandemic. OEI-02-20-00520. HHS Office of Inspector General. Published 2022. Accessed March 27, 2023. https://oig.hhs.gov/oei/reports/OEI-02-20-00520.asp
4. Katz AJ, Haynes K, Du S, Barron J, Kubik R, Chen RC. Evaluation of telemedicine use among US patients with newly diagnosed cancer by socioeconomic status. JAMA Oncol. 2022;8(1):161-163.
5. Weiner JP, Bandeian S, Hatef E, Lans D, Liu A, Lemke KW. In-person and telehealth ambulatory contacts and costs in a large US insured cohort before and during the COVID-19 pandemic. JAMA Netw Open. 2021;4(3):e212618.
6. Shaver J. The state of telehealth before and after the COVID-19 pandemic. Prim Care. 2022;49(4):517-530.
7. Totten AM, McDonagh MS, Wagner JH. The Evidence Base for Telehealth: Reassurance in the Face of Rapid Expansion During the COVID-19 Pandemic. White Paper Commentary. (Pacific Northwest Evidence-based Practice Center, Oregon Health & Science University under Contract No. 290-2015-00009-I). Rockville, MD: Agency for Healthcare Research & Quality;2020.
8. Yeramosu D, Kwok F, Kahn JM, Ray KN. Validation of use of billing codes for identifying telemedicine encounters in administrative data. BMC Health Serv Res. 2019;19(1):928.
9. US Centers for Medicare & Medicaid Services. Medicare Telemedicine Data Snapshot Methodology. US Centers for Medicare & Medicaid Services. Published 2022. Accessed March 27, 2023. https://www.cms.gov/files/document/medicare-telemedicine-snapshot-methodology.pdf
10. US Department of Health and Human Services Office of Inspector General. Medicare Telehealth Services During the First Year of the Pandemic: Program Integrity Risks. OEI-02-20-00720. Office of Inspector General. Published 2022. Accessed March 27, 2023. https://oig.hhs.gov/oei/reports/OEI-02-20-00720.pdf
11. Centers for Medicare & Medicaid Services. Place of Service Code Set: Place of Service Codes for Professional Claims. Centers for Medicare & Medicaid Services. Published 2021. Updated September 2021. Accessed March 27, 2023. https://www.cms.gov/Medicare/Coding/place-of-service-codes/Place_of_Service_Code_Set
12. Centers for Medicare & Medicaid Services. Medicare Telemedicine Health Care Provider Fact Sheet. Centers for Medicare & Medicaid Services. Published 2020. Updated March 17, 2020. Accessed March 27, 2023. https://www.cms.gov/newsroom/fact-sheets/medicare-telemedicine-health-care-provider-fact-sheet
13. Centers for Medicare & Medicaid Services. CMS Manual System. Department of Health & Human Services. Published 2022. Accessed March 27, 2023. https://www.cms.gov/files/document/r11437CP.pdf
14. Centers for Medicare & Medicaid Services. Restructured BETOS Classification System: Information that allows researchers to group Medicare Part B healthcare service codes into clinically meaningful categories and subcategories. Centers for Medicare & Medicaid Services. Published 2022. Updated October 20, 2022. Accessed March 27, 2023. https://data.cms.gov/provider-summary-by-type-of-service/provider-service-classifications/restructured-betos-classification-system