Logical Inconsistencies in the Health Years in Total and Equal Value of Life-Years Gained
Section Editor: Agnes Benedict
Paulden M, Sampson C, O’Mahony JF, et al. Value Health. 2024;27(3):356-366
The quality-adjusted life-year (QALY) has been the standard measure in economic evaluations and is used widely in many health technology assessment (HTA) countries for decision making. The use of QALY is subject to much criticism and an ongoing debate since its inception several decades ago. The controversy is reflected by the title of Milton Weinstein’s 1998 paper entitled, “A QALY Is a QALY Is a QALY—Or Is It?”1 The answer by many is that it is not. There is evidence that an improvement brought about for patients who generally have poor quality of life may be valued more by society than their healthier counterparts. However, since the same extension of life is weighted by a lower health utility, in the standard QALY framework that will not be true. Recent years have seen proposals for alternative approaches, including the equal value of life-years gained (evLYG)2 and “health years in total” (HYT).3 These are actively discussed by HTA bodies and evLYG calculation is considered by the Institute for Clinical and Economic Review. However, due to their recency, a lot less general knowledge and experience have been accumulated among members of the health economics and outcomes research (HEOR) community4 with these approaches, compared to the QALY approach.
The paper by Paulden and colleagues summarizes these new proposed methods and provides step-by-step illustrations of how to calculate both measures through simple examples that involve comparisons of mutually exclusive treatment options that can achieve 3 different life expectancies with different quality of life.
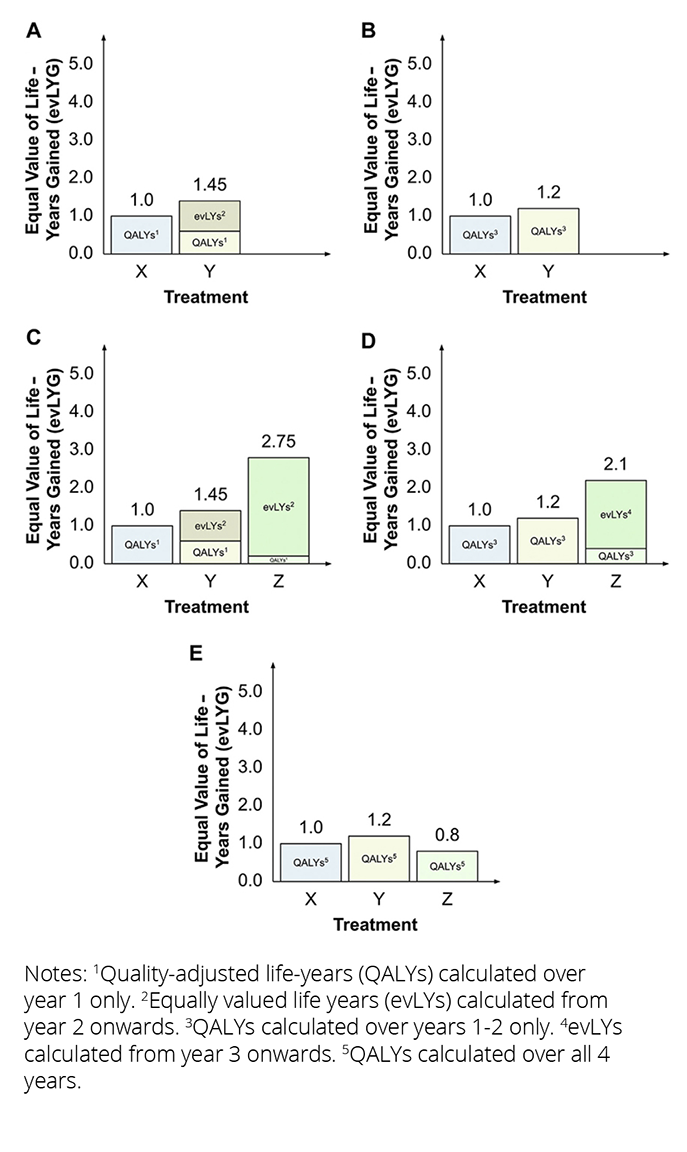
The paper then compares the 2 new approaches to each other and to the classic approach of comparing technologies using QALYs and life years only. The authors point to some logical inconsistencies in decision making by applying the new methods. The evLYG approach, the authors suggest, can result in decision instability, since the preferred decision depends on what is considered current standard of care. As illustrated in the Figure below, the choice among 3 therapies X, Y, and Z will depend on which one is considered standard of care. When only X and Y are available, Y is always preferred (panels A and B). When Z is the new treatment and either X or Y is standard of care, Z will be preferred (panels C and D). However, if Z becomes the standard of care and a reassessment takes place, preference ordering of the original 2 treatments may change (from Z to Y), as shown in panel E.
Figure. evLYG for each treatment, assuming (A) treatment Z is not available and treatment X is current treatment; (B) treatment Z is not available and treatment Y is current treatment; (C) treatment Z is available and treatment X is current treatment; (D) treatment Z is available and treatment Y is current treatment; or (E) treatment Z is available and treatment Z is current treatment.
The authors also show that the HYT violates the basic axiom of rational choice theory of “independence of irrelevant alternatives.” Under certain circumstances, if a new, mutually exclusive option of treatment C becomes available, the preferred choice between treatment A versus treatment B may change. This may result in inconsistent social decision making. Other important practical and theoretical concerns with the method of HYT are summarized, including (but not restricted to) its capacity to handle heterogeneity and the plausibility of separating the value of life expectancy and the value of a certain health-related quality of life.
The paper fills a gap for members of the HEOR community by providing an overview of the background to each proposal, by explaining and comparing the new approaches in easy-to-follow terms through some simple examples. The challenges with their applications are explained in terms of real situations HTAs may face. The paper then closes with a proposal for an alternative that is free of logical inconsistencies: that of equity-weighted QALYs that can address the original issue with the QALY-based approach, while meeting the axioms of rational decision making. The authors highlight that equity weighting is not straightforward to do properly and provide references to past research in the area. For anyone interested in this fundamental question in health economics, this paper is strongly recommended.
References
1. Weinstein MC. A QALY is a QALY—or is it? J Health Econ. 1988;7(3):289-290. doi: 10.1016/0167-6296(88)90030-6
2. Carlson JJ, Brouwer ED, Kim E, Wright P, McQueen RB. Alternative approaches to quality-adjusted life-year estimation within standard cost-effectiveness models: literature review, feasibility assessment, and impact evaluation. Value Health. 2020;23(12):1523-1533. doi: 10.1016/j.jval.2020.08.2092
3. Basu A, Carlson J, Veenstra D. Health years in total: a new health objective function for cost-effectiveness analysis. Value Health. 2020;23(1):96-103. doi: 10.1016/j.jval.2019.10.014
4. O’Day K, Mezzio DJ. Demystifying ICER’s equal value of life years gained metric. Value & Outcomes Spotlight. 2021;7(1):26-28. www.ispor.org/publications/journals/value-outcomes-spotlight/vos-archives/issue/view/overcoming-vaccine-hesitancy-injecting-trust-in-the-community/demystifying-icer-s-equal-value-of-life-years-gained-metric

