Health Equity for HTA:
A Conversation With Wanrudee Isaranuwatchai, PhD

Section Editor: Marisa Santos, PhD, MD, Instituto Nacional de Cardiologia, Rio de Janeiro, Brazil
Recently, I had the pleasure of interviewing Wanrudee Isaranuwatchai, PhD, Program Leader and Senior Researcher of the Health Intervention and Technology Assessment Program (HITAP) in Thailand. She is also an Affiliated Scientist at St. Michael’s Hospital and an Associate Professor at the Institute of Health Policy, Management, and Evaluation at the University of Toronto in Canada.
Dr Isaranuwatchai’s research focuses on how to apply health economics and health technology assessment (HTA) in the real-world setting as well as how to advance methods in economic evaluation. Her experience and keen interest in the potential use of big data in health economics and HTA to support evidence generation and the policy-making process make her an ideal person to share her perspective on this month’s theme of improving equity through HTA.
VOS: In recent years, the subject of health equity has gained popularity in HTA. What is causing so much interest in your point of view?
Wanrudee Isaranuwatchai: In the words of Nelson Mandela, “Health cannot be a question of income; it is a fundamental human right.” Health equity has always been an important topic in our society including in the field of HTA. Evolution of incorporating equity was reflected in the updated definitions of HTA.1 One could consider inequity as a long-standing challenge in our HTA field to have an approach that enables the consideration of health equity into economic evidence. Public health is about ensuring that no one is left behind while overall health improves.2 This goal is achieved through equitable access in healthcare, which is also a key feature of global health policy agendas and the universal health coverage movement. Therefore, many would consider equity to be one of the essential parts of public health policy.
Although recognizing that health inequity is a concern is a good first step, the COVID-19 pandemic brought forward the reality that talking about it will not address it.3 Many are recognizing that the long-standing socioeconomic inequities disproportionately affecting vulnerable and marginalized populations are now wider than ever, especially when there are public health emergencies. In our work to help identify best buys, wasted buys, and contestable buys for noncommunicable disease (NCD) prevention,4,5 the results identify several considerations to use when deciding whether and how to implement an NCD prevention intervention—and health equity was one of those considerations.
VOS: To what extent do HTA reports include pertinent information about equity issues? Do they actually alter how decisions are made in practice?
WI: There are movements to incorporate equity considerations as a part of HTA to support the policy- and decision-making process. Our team conducted a landscape analysis of HTA capacity in the Association of South-East Asian Nations region and identified that equity was a factor in the decision-making process for a few countries.6
Specifically in Thailand, several pieces of evidence are used to assist the policy makers before decisions are made on reimbursement for Universal Health Care Benefit Package and National List of Essential Medicines. Topic prioritization criteria include: (i) number of people affected by the disease or health problem; (ii) severity of the disease or health problem; (iii) effectiveness of the health technology; (iv) variation in practice; (v) impact on household expenditure; and (vi) equity, social, and ethical considerations. Meanwhile, decision-making criteria include: (i) cost-effectiveness; (ii) availability of clinical practice guidelines; (iii) health system readiness; (iv) budget impact; and (v) ethical and social issues. In both processes, the last component takes into consideration health equity before any decisions so that equity issues can influence how decisions are made in practice (as they should). Policy makers have also shown their interests and support to incorporate health inequity into the decision-making process, if possible, in a systematic and evidence-informed way. Engagement with stakeholders during the research process—including civil society in the board of the decision-making body—helps keep equity issues in sight. With that being said, the incorporation of health equity issues into economic evidence remains to be implemented.
In an ideal world, it would be easy and straightforward to prioritize and allocate resources to interventions that have the maximum impact on health, while ensuring fair and equitable distribution of resources to all and minimizing the risk of financial hardship from out-of-pocket payments. In the real world, however, things may be quite different. In our work on NCD prevention,4,5 we recognized that, clearly, what is best or wasted is more than just a question of effectiveness and cost. There are other ethical, cultural, political, and practical factors that are crucial and should be considered when making decisions.
VOS: How could cost-effectiveness analysis (CEA) research on the consequences for health equity be more impactful?
WI: It is one thing to know that it is important but another to do something about it. The first step perhaps would be to recognize when the topic we are doing a CEA on has an equity consideration that should be taken into account. Subsequently, the traditional CEAs should then be adapted to explicitly incorporate health equity considerations using one of the existing methods (eg, a distributional cost-effectiveness analysis [DCEA], an extended cost-effectiveness analysis [ECEA]) so that the findings will be comprehensive and useful to policy makers.
Reporting standards, such as Consolidated Health Economic Evaluation Reporting Standards (CHEERS), have recently updated thier guidelines to include criteria on health equity, highlighting the importance of health equity and how it should be incorporated (when relevant) to CEA research.7
VOS: What are the central concepts of health equity that cost-effectiveness research can access?
WI: The overall goal of DCEA (which incorporates health equity) aligns with CEA in that these methods aim to provide evidence to support the decision-making process, but not to make the decisions for policy makers. Traditional CEA tells us whether an intervention provides a good value-for-money (referring to the efficiency aspect). This exploration is done by examining the trade-offs between health effects and costs associated with the interventions. What it does not show is how these health outcomes and costs are distributed across different population groups of interest. DCEA and ECEA are specifically designed to: (i) identify these population groups (which can vary by the topics, diseases, or intervention being assessed); and (ii) distribute the costs and health effects by such groups. Therefore, DCEA and ECEA can tell us both whether an intervention is a good value-for-money and whether the intervention enhances or reduces health equity. As a result, we can see the trade-offs between the impact on efficiency and equity from an intervention. This approach is useful as it helps us choose interventions depending on the objective of improving total health versus improving equity. These objectives are generally set by policy makers, but they should reflect the overall preference and need of the society at a given time.
Information from such analyses can be used to support several types of decisions such as designing benefit healthcare packages, purchasing certain health interventions, investing in healthcare infrastructure, or supporting public health initiatives that enhance both equity and efficiency.8
“Real-world evidence has been the talk of the town for some time. It would be informative to see how real-world data could be used to support this appetite of data from methods such as DCEA and ECEA.” — Wanrudee Isaranuwatchai, PhD
VOS: How can health initiatives affect socially disadvantaged groups and vulnerable people differently? Can you give some real-world examples?
WI: Socially disadvantaged groups and vulnerable people face additional challenges more than others. Seeking only to maximize health benefits can conflict with equity.9 For example, achieving equity tends to become costlier as policy reaches out to less accessible, marginalized groups. At the same time, exclusion of hard-to-reach populations (including socially disadvantaged groups and vulnerable people) raises important ethical questions regarding a just distribution of access to healthcare and of health itself.
For example, DCEA has been used to assess the inequality impact of technologies recommended by National Institute of Health and Care Excellence in the United Kingdom between 2012 to 2014.10 Among the 27 interventions that were evaluated, 14 interventions were estimated to increase population health and reduce health inequality, 8 to reduce population health and increase health inequality, and 5 to increase health and increase health inequality. A DCEA in Ethiopia explored the equity impact of a hypothetical redesigned rotavirus vaccination program.11 The study found that diverting additional resources into vaccine delivery in rural areas resulted in not cost-effective but equity-enhancing outcomes and found the equity-efficiency trade-offs to be worthwhile given decision makers’ objective to reduce health inequity. Another study utilized ECEA to explore the consequences of tobacco tax on household health and finances among rich and poor smokers in China over a 50-year period.12 They found that such excise tax increase could be pro-poor in China as the years of life-year gained would be more concentrated on the poor (79 million in the poorest quintile group) than on the rich (11 million in the richest quintile group), and the financial risk-protection benefits would be largely concentrated among the poorest quintile group (accruing about 70% of the total $2 billion of insurance value gained).
In one of our works on NCDs,5 we found that every single day NCDs cause more than 100,000 deaths—80% of which occur in low- and middle-income countries.13 Additionally, mental health problems are the leading cause of disability around the world. For example, approximately 800,000 people commit suicide every year and about 75% of those occur in low- and middle-income countries (LMICs).14
We see and experience discrepancies in health in all levels, and the question remains, what are we going to do about it if we are to be at this crossroad of efficiency and equity? Another example (a common phenomenon globally) could be the considerations to publicly fund high-cost drugs that mostly are not cost-effective but could reduce inequity. Having evidence on the equity-efficiency trade-offs has potential to assist real-world decisions.
VOS: What exactly does “extended cost-effectiveness analysis” entail?
WI: ECEA is another approach to address health policy assessment by capturing equity within decision making. The distinguishing feature of ECEA from traditional CEA and DCEA is its emphasis on financial risk protection.15 ECEA helps analyze the distribution of both health benefits and financial risk protection benefits (prevention of illness-related impoverishment) per dollar expenditure for a specific policy, so this method is appropriate when policy makers are interested in examining the financial risk protection benefits of policies (where out-of-pocket payments may be high) and preventing medical impoverishment.
VOS: How might the net health benefits concept help to analyze the impact on equity?
WI: Net health benefit is another summary measure in HTA that aims to present the benefit in terms of health (rather monetary value) from the difference between the expected benefits of a decision and the expected associated opportunity costs.8 DCEA applies the concept of net health benefit at the equity-relevant variable level (ie, population groups of interest) rather than at the general population level (which assumes equal effect) to incorporate equity into analysis by analyzing the distribution of benefits and opportunity costs. The forgone health benefits that could have been generated through the next-best alternative may be unequally distributed, and this distribution is required to estimate the net distributional health impact of a program. Three key pieces of information will be needed for this analysis: (i) the baseline distribution of health; (ii) distribution of health opportunity costs; and (iii) distribution of health benefits. However, the use of net health benefit alone (metric for efficiency) is not enough to comprehend and measure the impact on equity.
VOS: What is the concept behind the equity trade-off?
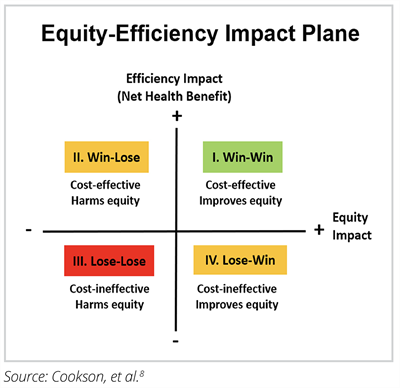
WI: HTA has often been criticized for its overemphasis on efficiency gains and lack of equity considerations in explicit forms. Traditional economic evaluations focus on the costs and effects of each intervention in an aggregated format. Impact of policies on equity can be measured using the DCEA approach by using metric that are of interest to policy makers. Reduction in an index of inequality in deprivation-related inequality in health-adjusted life expectancy has been used by researchers in England and Ethiopia to measure equity impact.
DCEA then utilizes combined information from net health benefit and equity impact to illustrate the underlying trade-offs between equity and efficiency as depicted by the equity-efficiency impact plane in Figure below. Interventions above the horizontal line are considered efficiency enhancing while those to the right of the vertical line are equity enhancing. This trade-off allows decision makers to keep their objectives in sight and in balance. In LMICs, vaccination and infectious disease control programs often fall into the northeast quadrant (enhancing both equity and efficiency), as they deliver large health gains per unit cost and disproportionately benefit socially disadvantaged groups. By contrast, investments in high-cost end-of-life treatments may fall into the southwest quadrant (reducing efficiency and widening equity gap) of being neither cost-effective nor likely to reduce social inequality in health. Hence, coverage of interventions in this quadrant will rely on other ethical and political arguments of value. In the northwest quadrant, the intervention is good for total health but bad for equity, and in the southeast quadrant, the option is bad for total health but good for equity. This can happen, for example, when socially disadvantaged groups gain less than advantaged groups from a decision to fund a medical technology, due perhaps to barriers to access, adherence, and long-term recovery, and additional investment in delivery infrastructure and follow-up care would be needed to facilitate equal access, adherence, and long-term recovery.
Figure.
VOS: What priority research is required at the intersection of equity and HTA?
WI: There are now methods (eg, ECEA, DCEA) available to incorporate equity into economic evaluations (a part of HTA). Perhaps the priority now is to apply these methods to the real-world case studies (at least that is what we are trying to do in Thailand in collaboration with partners in United Kingdom and Singapore). A case study to show how innovative methods such as DCEA can assist in the decision-making process in the real world can illustrate the future of improved decision-making processes that explicitly and systematically consider health equity. This first case study of DCEA in Thailand will illustrate how equity considerations can be formally analyzed and incorporated into decision making. This study can equip decision makers with the tools to improve health equity as well as comprehend the implications of prioritizing health programs solely based on efficiency gains. More importantly, this type of analysis can provide policy makers with information on how to design and implement an equity enhancing health intervention.
VOS: What are the primary obstacles to implementing these ideas?
WI: DCEA is a data-hungry method and it may not be possible to collect all relevant socioeconomic parameters (relevant to equity issues) in a study. We may only determine a few dimensions to incorporate equity considerations in CEA, which is largely dependent on the level of data that may be available. To mitigate this challenge, research teams should explore data from local contexts whenever possible, including the options of exploring expert elicitation and consulting international literature to obtain data for model parameters.
Furthermore, real-world evidence has been the talk of the town for some time. It would be informative to see how real-world data (RWD) could be used to support this appetite of data from methods such as DCEA and ECEA. Our network in Asia recognizes the potential of RWD and came together to create a nonbinding document to support the use of RWD.16 However, for RWD to truly fulfill its potential to help address important issues such as health equity, different stakeholders (including governments, private sector, academics, and the public) must find harmony and balance in sharing big data while protecting data privacy.
References
1. O’Rourke B, Oortwijn W, Schuller T. The new definition of health technology assessment: a milestone in international collaboration. Int J Technol Assess Health Care. 2020;36(3);187-190.
2. Galea S. Race, history, and the science of health inequities. Boston University School of Public Health website. Published 2019. Accessed July 27, 2022. https://www.bu.edu/sph/news/articles/2019/race-history-and-the-science-of-health-inequities
3. Ten billion COVID vaccinations: world hits new milestone. Nature website. Published January 31, 2022. Accessed July 27, 2022. https://www.nature.com/articles/d41586-022-00285-2
4. Isaranuwatchai W, Teerawattananon Y, Archer RA, et al. Prevention of non-communicable disease: best buys, wasted buys, and contestable buys. BMJ. 2020:368:m141. https://doi.org/10.1136/bmj.m141
5. HiTAP website. Accessed July 27, 2022/. https://www.buyitbestncd.health/
6. Sharma M, Teerawattananon Y, Dabak, et al. A landscape analysis of health technology assessment capacity in the Association of South-East Asian Nations region. Health Res Policy Sys. 2021;(19):19. https://doi.org/10.1186/s12961-020-00647-0
7. Husereau D, Drummond M, Augustovski F, et al. Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) Explanation and Elaboration: A report of the ISPOR CHEERS II Good Practices Task Force. Value Health. 2022;25(1):10-31.
8. Cookson R, Griffin S, Norheim OF, Culyer AJ. Distributional Cost-Effectiveness Analysis Quantifying Health Equity Impacts and Trade-Offs: Quantifying Health Equity Impacts and Trade-Offs. Oxford, UK: Oxford University Press; 2020.
9. Rumbold B, Baker R, Ferraz O, et al. Universal health coverage, priority setting, and the human right to health. Lancet. 2017;390:712-714. https://doi.org/10.1016/S0140-6736(17)30931-5
10. Love-Koh J, Cookson R, Gutacker N, Patton T, Griffin S. Aggregate distributional cost-effectiveness analysis of health technologies. Value Health. 2019;22(5):518-26.
11. Dawkins BR, Mirelman AJ, Asaria M, Johansson KA, Cookson RA. Distributional cost-effectiveness analysis in low- and middle-income countries: illustrative example of rotavirus vaccination in Ethiopia. Health Policy Plan. 2018;33(3):456-463.
12. Verguet S, Gauvreau CL, Mishra S, et al. The consequences of tobacco tax on household health and finances in rich and poor smokers in China: an extended cost-effectiveness analysis. Lancet Glob Health. 2015;3(4):206-216. https://doi.org/10.1016/s2214- 109x(15)70095-1
13. Non-communicable diseases. World Health Organization website. Published 2018. Accessed July 26, 2022. https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases
14. 10 Factors on Mental Health. World Health Organization website. Published 2019. Accessed July 27, 2022. https://www.who.int/features/factfiles/mental_health/mental_health_facts/en/index1.html
15. Verguet S, Laxminarayan R, Jamison DT. Universal public finance of tuberculosis treatment in India: an extended cost-effectiveness analysis. Health Econ. 2015;24(3):318-332.
16. Lou J, KC S, Toh YK, et al. Real-world data for health technology assessment for reimbursement decisions in Asia: current landscape and a way forward. Int J Technol Assess Health Care. 2020;36:474-480. https://doi.org/10.1017/S0266462320000628